Opioid-Induced Testosterone Estimator
Estimate Your Testosterone Levels
This tool estimates your testosterone levels based on the opioid you're taking and your daily dose. The World Health Organization's normal range for adult males is 270-1040 ng/dL.
Key Takeaways
- Long‑term opioid use can suppress the hypothalamic‑pituitary‑gonadal (HPG) axis, leading to opioid‑induced androgen deficiency (OPIAD).
- Common signs include low libido, erectile dysfunction, fatigue, mood changes, loss of muscle mass and increased fracture risk.
- Screening with morning testosterone tests and symptom questionnaires is essential for anyone on opioids >90 days.
- Testosterone replacement therapy (TRT) improves sexual function, body composition and may cut mortality risk.
- Non‑pharmacologic measures - weight control, resistance exercise, sleep hygiene - help support testosterone while on opioids.
When patients stay on opioids for chronic pain or opioid agonist therapy, they often notice a drop in energy, mood, or sexual desire. Those changes aren’t just “side effects” - they’re the hallmark of opioid‑induced androgen deficiency (OPIAD), also called opioid‑induced hypogonadism. Understanding how opioids mess with hormone production, spotting the warning signs, and knowing the safest ways to restore testosterone can dramatically improve quality of life.
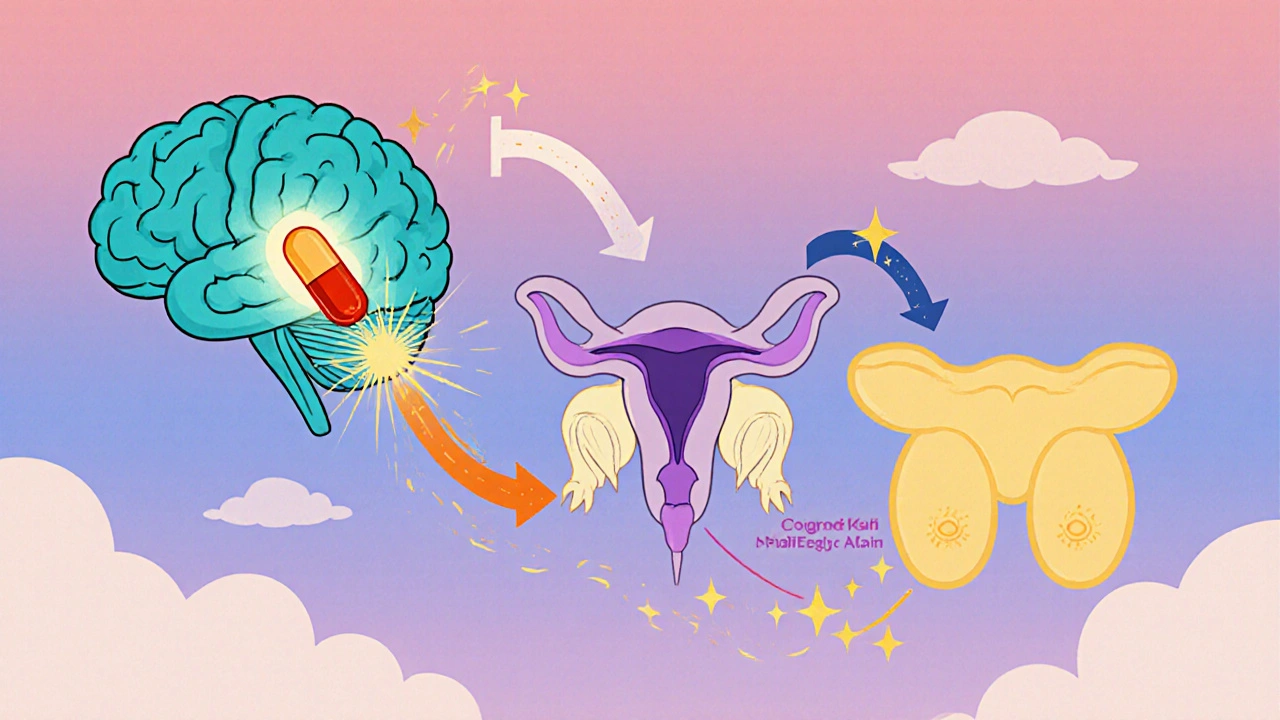
How Opioids Disrupt Testosterone Production
Opioids bind to mu‑opioid receptors in the hypothalamus. This dampens the pulsatile release of gonadotropin‑releasing hormone (GnRH). With less GnRH, the pituitary gland cuts back on luteinizing hormone (LH), and the testes receive a weaker signal to make testosterone. The cascade is known as suppression of the hypothalamic‑pituitary‑gonadal (HPG) axis.
Research shows a clear dose‑response relationship: patients on opioids for more than 90 days have testosterone levels 35‑50 % lower than baseline, and those on therapy for over a year can drop 50‑75 % (Pain Physician 2012). Long‑acting agents such as methadone or buprenorphine produce deeper suppression than short‑acting heroin because the former maintain steadier receptor activation.
Who’s at Risk?
The prevalence estimates vary wildly-studies report 50‑90 % of long‑term opioid users develop some degree of hypogonadism. The World Drug Report 2023 counted 58 million opioid users worldwide in 2022, implying millions could be living with OPIAD unnoticed.
Key risk factors include:
- Duration of therapy >90 days
- Higher daily morphine‑equivalent dose
- Use of long‑acting formulations (methadone, buprenorphine, extended‑release oxycodone)
- Older age (testosterone naturally declines, making the drop more pronounced)
- Concurrent conditions that already lower testosterone - obesity, diabetes, chronic liver disease
Recognising the Symptoms
Symptoms fall into two buckets: sexual‑function changes and systemic effects.
Sexual signs (reported in 68‑85 % of affected males) include:
- Low libido
- Erectile dysfunction (60‑75 % prevalence)
- Reduced spontaneous erections
Systemic signs are less specific but equally debilitating:
- Chronic fatigue (fatigue severity scores 2.5 × higher than normals)
- Irritability and depressed mood (40 % higher depression scores)
- Poor concentration and memory lapses
- Loss of muscle mass, increased visceral fat
- Osteoporosis - lumbar spine BMD down 15‑20 %
- Mild anemia (average hemoglobin ≈ 12.3 g/dL)
Because many of these complaints overlap with chronic pain itself, clinicians must keep a high index of suspicion, especially when symptoms emerge 3‑6 months after starting continuous opioid therapy.
Screening & Diagnosis
Guidelines recommend a two‑step approach:
- Administer a symptom questionnaire such as the Androgen Deficiency in Aging Males (ADAM) tool. Three or more positive answers trigger lab work.
- Measure total and free testosterone between 7‑10 AM on two separate mornings. Values <300 ng/dL are generally considered low for adult men.
For women on opioids, clinicians may consider dehydroepiandrosterone (DHEA) levels, though evidence is thinner.
Treatment Options
Once OPIAD is confirmed, the mainstay of therapy is testosterone replacement therapy (TRT). Delivery methods differ in convenience, cost, and side‑effect profile.
| Formulation | Typical Dose | Frequency | Key Advantages |
|---|---|---|---|
| Testosterone cypionate (IM) | 100‑200 mg | Every 1‑2 weeks | Reliable serum levels; widely available |
| Testosterone enanthate (IM) | 100‑200 mg | Every 1‑2 weeks | Similar to cypionate; flexible dosing |
| Transdermal gel | 50‑100 mg (applied daily) | Once daily | Non‑invasive; avoids injection pain |
| Transdermal patch | 5‑7.5 mg | Once daily | Steady release; easy removal |
| Buccal tablet | 30 mg | Twice daily | Bypasses liver first‑pass metabolism |
Clinical trials in chronic non‑cancer pain patients show TRT improves International Index of Erectile Function scores from 12.5 to 19.8, adds ~3.2 kg lean mass and reduces fat mass by ~2.1 kg over 6 months. Moreover, a JAMA Network Open 2019 cohort linked TRT to a 49 % lower all‑cause mortality and fewer major cardiac events.
Monitoring During TRT
After starting therapy, repeat testosterone labs at 3‑6 months, aiming for 350‑750 ng/dL. Yearly checks should include:
- Hematocrit (watch for polycythemia; >54 % may need phlebotomy)
- PSA and digital rectal exam in men >50 or with prostate risk factors
- Lipid panel (TRT can lower HDL by 10‑15 mg/dL)
- Blood pressure and cardiovascular review
Any rise in PSA >0.4 ng/mL/year or sudden worsening of urinary symptoms warrants endocrinology referral.
When TRT Is Not Appropriate
Contraindications mirror those in standard endocrinology guidelines:
- Active or high‑risk prostate or breast cancer
- Uncontrolled severe heart failure
- Recent thromboembolic event (relative risk of VTE rises 1.4‑2.0× with testosterone)
If risks outweigh benefits, clinicians can focus on lifestyle optimisation and consider aromatase inhibitors or selective estrogen receptor modulators only in specialist settings.
Non‑Pharmacologic Strategies to Boost Testosterone
Even while on opioids, patients can adopt habits that naturally nudge testosterone upward:
- Weight management: BMI < 25 correlates with 20‑30 % higher levels.
- Resistance training: 3 sessions/week raise testosterone by 15‑25 %.
- Sleep hygiene: 7‑9 h/night supports a 20 % increase.
- Avoid tobacco and excess alcohol: Smoking cuts testosterone 15‑20 %; >14 drinks/week drops it 25 %.
- Control blood sugar: Diabetes patients show 25‑35 % lower testosterone.
These measures are especially valuable for patients who cannot receive TRT or who wish to minimise medication exposure.
Comparing Opioid Types and Their Impact on Testosterone
| Opioid | Typical Daily Dose (MME) | Mean Testosterone | Notes |
|---|---|---|---|
| Methadone (maintenance) | 80‑120 | 245 | Long‑acting, strongest HPG suppression |
| Buprenorphine | 8‑16 | 387 | Partial agonist, milder suppression |
| Extended‑release oxycodone | 40‑100 | 310‑350 | Dose‑dependent decline |
| Intrathecal morphine | Variable | ~260 | Rapid suppression noted in controlled studies |
These numbers illustrate why clinicians often screen methadone‑treated patients first.
Practical Steps for Clinicians
- Identify patients on opioids >90 days or on long‑acting formulations.
- Use the ADAM questionnaire during routine visits.
- Obtain two morning total testosterone levels; add free testosterone if total is borderline.
- If low, discuss TRT options, review contraindications, and obtain informed consent.
- Start with the least invasive formulation the patient prefers; schedule lab follow‑up at 3 months.
- Document symptom changes using the International Index of Erectile Function (IIEF) and pain scores.
- Coordinate care with endocrinology for complex cases or men over 50 with prostate concerns.
Embedding this workflow into electronic medical records can improve detection rates, which historically sit below 10 % despite high prevalence.
Future Directions & Gaps in Knowledge
Although recent data are promising, several questions linger:
- Large‑scale, prospective cohort studies are needed to define optimal screening intervals.
- Long‑term safety of TRT in opioid users-especially cardiovascular outcomes-remains under‑studied.
- Effects of newer opioid formulations (e.g., abuse‑deterrent OxyContin) on the HPG axis are unclear.
- Research on female OPIAD and potential role of DHEA or selective androgen receptor modulators is sparse.
Addressing these gaps will help refine guidelines and improve patient outcomes as the opioid landscape continues to evolve.
Bottom Line
If you or a loved one is on chronic opioids and notice a dip in energy, mood, or sexual health, ask your doctor to check testosterone. Early detection and appropriate treatment-whether TRT, lifestyle changes, or a switch to a less suppressive opioid-can restore vitality and may even lower the risk of serious complications.
What is opioid‑induced androgen deficiency (OPIAD)?
OPIAD is a hormone disorder caused by prolonged opioid use that suppresses the hypothalamic‑pituitary‑gonadal axis, leading to low testosterone levels and related symptoms.
How soon after starting opioids can testosterone drop?
Significant declines can appear within 3‑6 months of continuous therapy, especially with long‑acting agents like methadone.
Which opioid carries the highest risk for low testosterone?
Methadone maintenance therapy shows the lowest average testosterone (≈245 ng/dL) compared with buprenorphine (≈387 ng/dL) and other opioids.
Is testosterone replacement safe for opioid users?
When monitored correctly, TRT improves symptoms and may lower mortality. Contraindications include prostate or breast cancer, uncontrolled heart failure, and recent clotting events.
Can lifestyle changes help without medication?
Yes. Maintaining a healthy weight, resistance training, adequate sleep, and avoiding tobacco/alcohol can raise testosterone by 15‑30 % and mitigate OPIAD effects.