Many people assume that if they have long-term care insurance, it will pay for everything that happens when they move into a nursing home - including their daily medications. But that’s not true. Long-term care insurance doesn’t cover prescription drugs, not even generic ones. This misunderstanding causes real problems for families trying to plan for care, and it leads to unexpected bills, delays in medication, and even skipped doses.
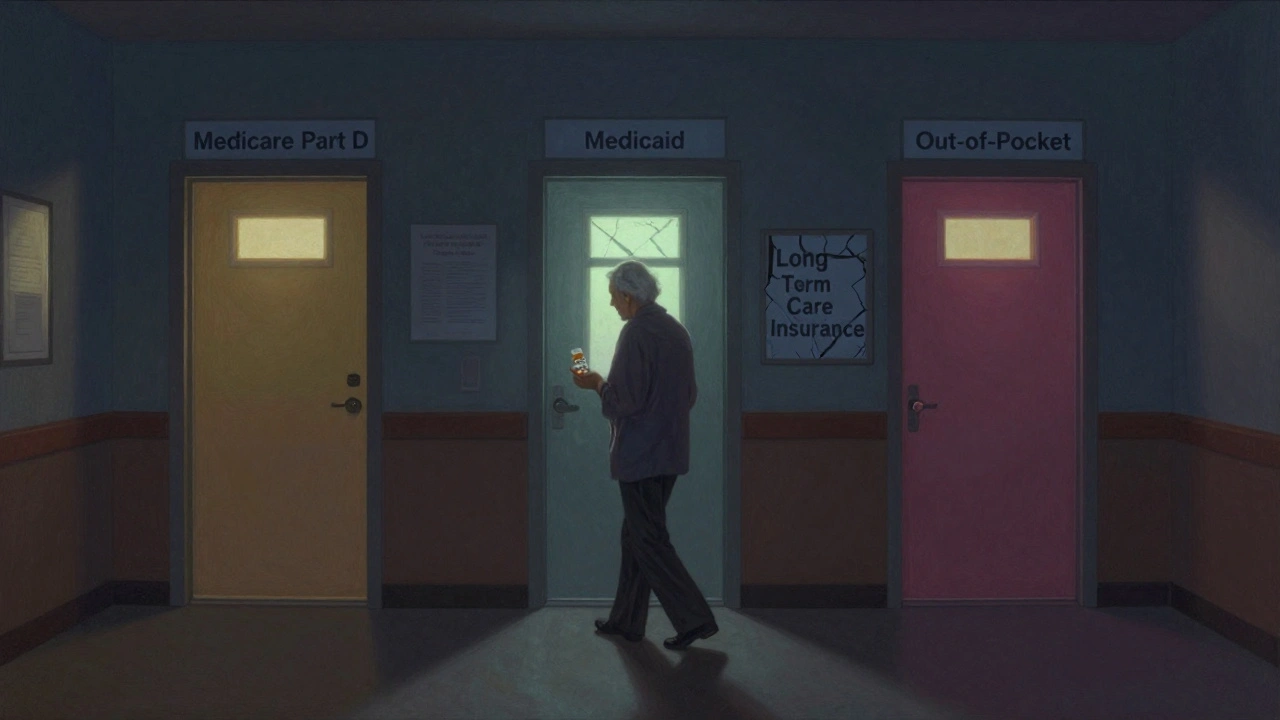
Think about it: if you’re in a nursing home, you’re likely taking multiple pills every day - blood pressure meds, diabetes drugs, cholesterol pills, maybe antibiotics or pain relievers. Most of these are generics, cheaper versions of brand-name drugs that work just as well. But who pays for them? Not your long-term care policy. That’s a common myth. Instead, your drug coverage comes from somewhere else - usually Medicare Part D, Medicaid, or out-of-pocket cash.
Why Long-Term Care Insurance Doesn’t Cover Drugs
Long-term care insurance was never meant to be health insurance. It was designed to pay for the cost of daily help - bathing, dressing, eating, moving from bed to chair - the kind of support people need when they can’t live independently anymore. That’s called custodial care. It’s not medical treatment. It’s personal care.
Prescription drugs are medical care. And medical care? That’s covered by health insurance, not long-term care insurance. The California Department of Insurance and Triage Health both confirm this clearly: even if your policy pays for your room, meals, and staff assistance in a nursing home, your pills are a separate bill.
This isn’t new. The separation has been in place since the 1970s, when long-term care insurance first became available. It got even clearer in 2006, when Medicare Part D launched. That’s when the federal government stepped in to handle prescription drug coverage for seniors, making it even more obvious that long-term care policies shouldn’t be expected to pay for meds.
Who Actually Pays for Generic Drugs in Nursing Homes?
If not long-term care insurance, then who? The answer depends on your situation, but here’s the breakdown:
- Medicare Part D covers about 82.4% of all prescription drugs in nursing homes. This is the biggest player. If you’re on Medicare and live in a nursing home, your drugs are likely paid through a Part D plan you enrolled in - either through a standalone plan or a Medicare Advantage plan.
- Medicaid pays for drugs for residents who qualify based on income. In these cases, Medicaid usually pays the pharmacy directly at acquisition cost plus a small dispensing fee.
- Private insurance (like an employer plan) covers about 8.5% of prescriptions. But many people lose this coverage once they enter a nursing home.
- Out-of-pocket - and this is the scary part - about 8.9% of nursing home residents pay for all their drugs themselves. That’s nearly 1 in 10 people.
Generics make up about 90% of the prescriptions written in nursing homes. They’re cheaper, safer, and just as effective as brand-name drugs. But even though they’re low-cost, if you don’t have coverage, paying for 10 or 15 generic pills a day adds up fast. A month’s supply of common generics can cost $150-$400. For someone on a fixed income, that’s a huge burden.
How Medicare Part D Works in Nursing Homes
Medicare Part D isn’t one plan. It’s hundreds of different plans offered by private companies like UnitedHealthcare, Humana, and CVS Health. Each plan has its own formulary - a list of drugs it covers. And not all formularies are the same.
Here’s the catch: even if a drug is FDA-approved and widely used, your Part D plan might not cover it. Or it might cover it only after you’ve tried another drug first. Or it might require your doctor to file paperwork to get approval. This is called a prior authorization.
Nursing homes have to track which plan each resident is on, check if their pharmacy works with that plan, and make sure the drugs are on the formulary. If a drug isn’t covered, the facility has to help the resident or their family request an exception. That process can take days - sometimes weeks. During that time, the resident might not get their medication.
A 2020 study found that residents without Part D coverage got significantly fewer prescriptions than those who had it. That’s not just inconvenient - it’s dangerous. Skipping meds for heart disease, diabetes, or mental health conditions can lead to hospitalizations, falls, or worse.
The Administrative Nightmare for Nursing Homes
Managing drug coverage isn’t just a problem for residents - it’s a nightmare for nursing homes. Before Part D, Medicaid handled drug payments in a single system. Now, facilities have to juggle dozens of different plans, each with different rules, formularies, and billing procedures.
A 2019 survey found that nursing homes spend 10 to 15 hours a week just managing drug coverage issues. That’s over 700 hours a year per facility. And it costs about $28,500 in staff time annually.
Some facilities have hired dedicated pharmacy liaisons or use electronic systems that connect to multiple Part D plans. These tools help reduce delays - cutting average wait times for medications from 3.2 days down to 0.7 days. But not every facility can afford that. Rural homes struggle even more. About 22% of rural nursing homes report trouble finding pharmacies that work with all the major Part D plans.
What About the Donut Hole and Out-of-Pocket Caps?
The Medicare Part D “donut hole” - a gap where you pay more after reaching a certain spending limit - used to be a big problem. But the Inflation Reduction Act of 2022 changed that. Starting in 2025, Medicare will cap out-of-pocket drug costs at $2,000 per year for all Part D enrollees. That’s huge for nursing home residents who rely on multiple medications.
Also, as of 2021, CMS requires Part D plans to cover all drugs on the official Medicare Part D Formulary and to approve non-formulary drug requests for nursing home residents within 72 hours. That’s a step forward. But it’s not foolproof. Some plans still drag their feet, and not all facilities know how to push back.
What Should You Do?
If you or a loved one is entering a nursing home, here’s what to do right now:
- Don’t assume your long-term care insurance pays for drugs. It doesn’t. Know that upfront.
- Confirm Medicare Part D enrollment. If you’re on Medicare, make sure you’re enrolled in a Part D plan. If you’re not, you might be paying full price for meds.
- Ask about the formulary. Find out which drugs your plan covers. Ask the nursing home’s pharmacy or social worker for a copy of the formulary. If a needed drug isn’t on it, ask about the exception process.
- Check for Medicaid eligibility. If income is low, Medicaid may cover drugs - and sometimes even long-term care costs.
- Use generic drugs whenever possible. They’re cheaper, equally effective, and most plans give you the lowest copay for them.
- Keep a list of all medications. Bring it with you to the nursing home. Include doses, reasons, and any allergies.
Many families don’t realize how complex this system is until they’re in the middle of a crisis. Planning ahead saves stress, money, and health.
What’s Changing in the Future?
By 2028, Medicare Part D is projected to cover 85.2% of nursing home drug costs - up from 82.4%. Out-of-pocket spending is expected to drop to 6.3%. That’s good news.
But challenges remain. Formulary restrictions still block access to needed drugs. Rural areas still struggle with pharmacy access. And many residents still fall through the cracks - especially those who don’t understand the system or can’t advocate for themselves.
The bottom line? Long-term care insurance is a valuable tool for covering the cost of daily care. But it’s not a health insurance replacement. For drugs, you need a different plan - and you need to know what it is before you need it.
Does long-term care insurance cover generic drugs in nursing homes?
No. Long-term care insurance covers custodial care - help with bathing, dressing, eating, and mobility - but it does not cover prescription drugs, including generics. Drug costs are covered by Medicare Part D, Medicaid, private insurance, or out-of-pocket payments.
Who pays for prescription drugs if I live in a nursing home?
Most often, Medicare Part D pays for drugs in nursing homes, covering about 82.4% of prescriptions. Medicaid covers drugs for low-income residents, and private insurance covers about 8.5%. About 8.9% of residents pay out-of-pocket because they lack coverage.
Why are generic drugs important in nursing homes?
Generic drugs make up 90% of prescriptions in nursing homes because they’re just as effective as brand-name drugs but cost much less. Most insurance plans give you the lowest copay for generics, making them the best choice for affordability and access.
What is a formulary, and why does it matter?
A formulary is a list of drugs that a Medicare Part D plan covers. If your medication isn’t on the list, you might not get it - or you might have to pay full price. Nursing homes must check your plan’s formulary to make sure your drugs are covered, and help you request exceptions if needed.
Can I switch my Medicare Part D plan after moving into a nursing home?
Yes. You can change your Part D plan during the Annual Enrollment Period (October 15 to December 7) or during a Special Enrollment Period if you move into a nursing home. It’s important to review your plan’s formulary and pharmacy network to ensure your drugs are covered.
What happens if my drug isn’t covered by my Part D plan?
Your nursing home or pharmacy can request an exception from your plan. For nursing home residents, CMS requires plans to respond within 72 hours. If denied, you can appeal. Some plans also allow temporary access to non-formulary drugs for up to 180 days.
Will the $2,000 out-of-pocket cap in 2025 help nursing home residents?
Yes. Starting in 2025, Medicare Part D beneficiaries will pay no more than $2,000 per year out-of-pocket for all prescription drugs. This will protect nursing home residents from high costs, especially those taking multiple medications daily.

