Every time you pick up your prescription, you might get a different pill. Same active ingredient. Different color. Different shape. Different brand name on the bottle. That’s not a mistake - it’s the new normal. In 2026, more than 90% of prescriptions in the U.S. are filled with generic drugs. And with so many manufacturers making the same medicine, your pharmacist may switch you between them without telling you. For most people, this works fine. For others, it can cause serious problems.
Why Do Generic Switches Happen?
Generic drugs are cheaper versions of brand-name medicines. Once a patent expires, multiple companies can make the same drug. They all have to prove they deliver the same active ingredient as the original. But here’s the catch: the law only requires them to be within 80% to 125% of the brand’s performance. That means one generic could be 20% weaker than the brand, and another could be 25% stronger. Put those two generics side by side, and they could differ by nearly 45% in how much medicine your body actually gets. This isn’t a flaw in the system - it’s how it’s designed. Insurance companies and pharmacies push for the cheapest option. If Teva’s version costs $5 and Mylan’s costs $7, the pharmacy will usually pick Teva. Then next month, if Mylan drops to $4, they switch again. It’s all about cost, not your body’s response.When Switching Can Be Dangerous
Not all drugs are created equal. Some have what’s called a narrow therapeutic index - meaning the difference between a helpful dose and a harmful one is tiny. For these, even small changes in how much medicine you get can cause big problems. Three of the most common drugs in this group are:- Levothyroxine (for hypothyroidism): A small drop in hormone levels can leave you exhausted, gain weight, or feel depressed. A small rise can cause heart palpitations or bone loss. Patients report feeling awful every time their pharmacy switches brands. One woman on Drugs.com said: “Every time my levothyroxine changes, my TSH goes out of range. I’m tired for weeks until my doctor adjusts my dose.”
- Warfarin (a blood thinner): Too little and you risk a clot. Too much and you could bleed internally. The FDA recommends staying on the same generic version for life. Yet, many patients get switched without warning. Studies show INR levels - which measure blood thinning - can swing wildly after a switch.
- Antiepileptic drugs (like phenytoin or lamotrigine): For people with epilepsy, even a 10% drop in blood levels can trigger a seizure. One Reddit user shared: “I switched from Mylan to Teva. Two weeks later, I had two breakthrough seizures. My neurologist checked my levels - they had dropped 30%.”
What You Might Not Notice - But Should
Most people don’t realize how often they’re being switched. Why? Because they don’t look at the pill. In a 2022 survey, 67% of patients identified their meds by how they looked - color, shape, imprint. When those change, they think it’s the same drug. But it’s not. This leads to real dangers:- Medication duplication: One in nine patients accidentally take two different generics of the same drug because they didn’t recognize the change.
- Adherence drops: If your pill looks different every time, you’re more likely to skip doses or get confused.
- Side effects appear: Some people report new headaches, dizziness, or nausea after a switch - not because the drug is bad, but because their body reacted to a new filler or coating.

Who’s Most at Risk?
It’s not just about the drug - it’s about you. Certain groups are far more likely to be affected:- Older adults: Often take multiple meds. Harder to track changes.
- People with chronic conditions: Heart disease, epilepsy, thyroid disorders, transplant recipients.
- Those on multiple generics: If you’re on five different generics, you’re getting switched five times a month.
- Patients with mental health conditions: Switching antidepressants or antipsychotics can cause relapse or worsening symptoms.
What You Can Do
You don’t have to accept random switches. Here’s how to take control:- Ask your pharmacist: “Is this the same manufacturer as last time?” Write down the name on the bottle - Teva, Mylan, Sandoz, etc.
- Request a specific generic: If you’ve had no issues with one brand, ask your doctor to write “Dispense as written” or “Do not substitute” on your prescription. This legally blocks the pharmacist from switching without approval.
- Use the same pharmacy: Chain pharmacies often switch manufacturers to save money. Independent pharmacies are more likely to keep your preferred version on hand.
- Monitor your symptoms: Keep a simple log. Note how you feel each week. If you start feeling off after a refill, check the manufacturer. Correlation isn’t proof - but it’s a clue.
- Get blood tests if needed: For drugs like warfarin, levothyroxine, or tacrolimus, ask your doctor to check your levels 2-4 weeks after any switch.
What Doctors and Pharmacists Should Be Doing
Many providers don’t realize how often switches happen. A 2023 survey found 62% of doctors didn’t know their patients had been switched until the patient came in with problems. Leading clinics now use “lock-in” programs for high-risk drugs. For example, a transplant center might only use one brand of tacrolimus for all their patients. That’s not just smart - it’s life-saving. Pharmacists are supposed to counsel patients on changes. But with high volumes and low pay, that often doesn’t happen. You have to be your own advocate.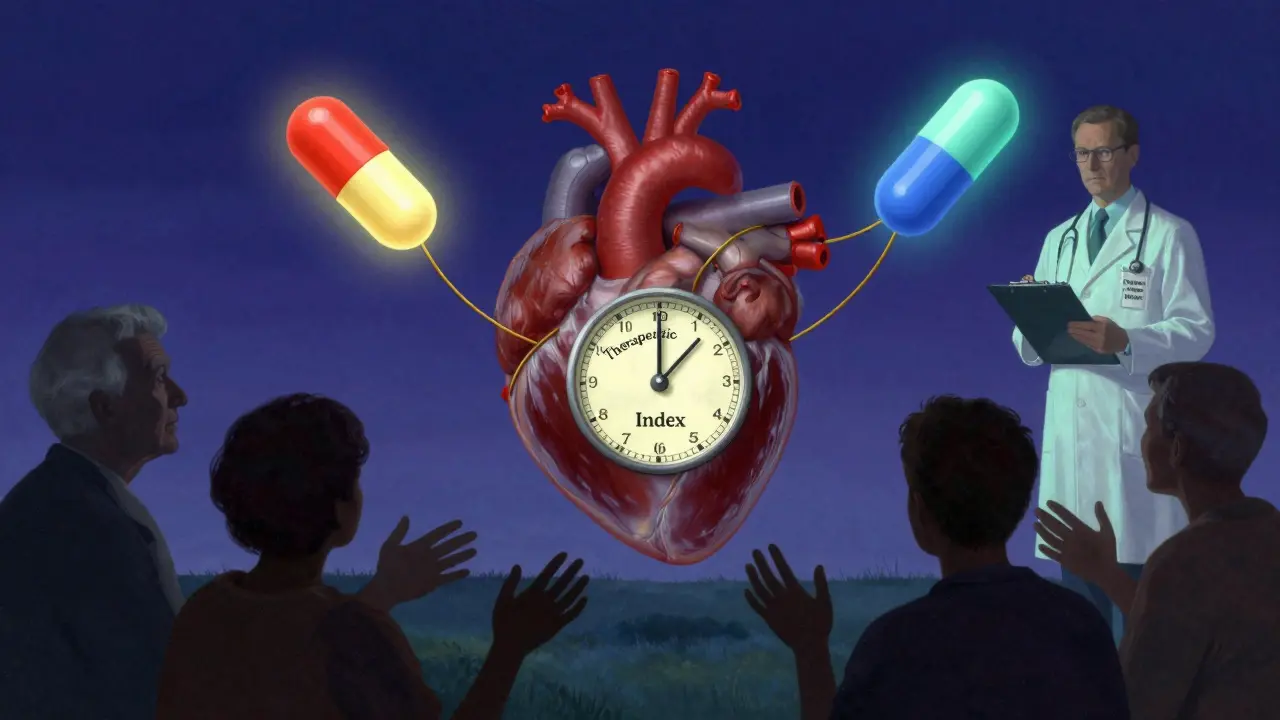
The Bigger Picture
The generic drug industry saved U.S. patients $8-10 billion in 2023. That’s huge. But the system is built for cost, not care. Companies compete on price, not consistency. And patients pay the price - sometimes with their health. The FDA is starting to pay attention. In 2024, they launched a pilot program requiring generic makers to report any formulation changes. Some states are pushing for mandatory labeling of manufacturers on prescriptions. But until then, the burden is on you.When Switching Is Fine
Don’t panic. For many drugs, switching causes zero issues. Statins (like atorvastatin), blood pressure meds (like lisinopril), and antibiotics (like amoxicillin) are very forgiving. One patient on GoodRx said: “I’ve had six different generics of lisinopril over five years. My blood pressure never budged.” If you’re on one of these, and you feel fine - keep taking it. No need to fix what isn’t broken.Bottom Line
Generic drugs are safe, effective, and essential. But assuming they’re all identical is dangerous. For some medicines - especially those with narrow therapeutic windows - switching between manufacturers isn’t harmless. It’s a risk. Your body doesn’t care about the price tag. It cares about the dose. And if that dose changes without you knowing, it can hurt. Know your drug. Know your manufacturer. Speak up. You’re not being difficult - you’re being smart.Can I ask my pharmacist to keep me on the same generic brand?
Yes. You can ask your doctor to write “Dispense as written” or “Do not substitute” on your prescription. This legally stops the pharmacy from switching you to another generic without calling your doctor first. You can also ask your pharmacist to order your preferred brand if it’s available.
Why do generic pills look different every time?
Each manufacturer uses different inactive ingredients - fillers, dyes, coatings - to make their version. The law doesn’t require generics to look like the brand or each other. So if you get Teva one month and Mylan the next, the color, shape, or imprint will change. That’s normal - but it can cause confusion.
Are generic drugs less effective than brand-name ones?
For most drugs, yes - they’re just as effective. The FDA requires generics to meet the same standards for safety and strength. But for drugs with a narrow therapeutic index - like levothyroxine, warfarin, or seizure meds - small differences in absorption or release can lead to real clinical effects. It’s not that generics are bad - it’s that they’re not always identical.
Should I avoid generics altogether?
No. Generics are safe, affordable, and responsible. Over 90% of prescriptions are filled with them. The issue isn’t generics - it’s unmonitored switching between multiple manufacturers. If you’re on a low-risk drug like statins or antibiotics, switching is usually fine. For high-risk drugs, stick with one manufacturer and monitor your response.
What should I do if I feel worse after a generic switch?
First, check the pill - is the manufacturer different? If yes, note the name. Then call your doctor or pharmacist. For high-risk drugs, ask for a blood test to check your levels. Don’t assume it’s “all in your head.” Many patients have had their symptoms confirmed by lab results after a switch. Your experience matters.
Is there a list of drugs that shouldn’t be switched?
Yes. Common ones include levothyroxine, warfarin, phenytoin, carbamazepine, cyclosporine, tacrolimus, and lithium. These have narrow therapeutic indexes. Medsafe and the FDA recommend avoiding switches for these drugs when possible. Ask your pharmacist or doctor for a full list based on your medications.

