If you’ve ever lain in bed at night feeling like your legs are crawling, tingling, or aching-and you just have to move them to make it stop-you’re not alone. About 1 in 10 adults in the U.S. and Europe deal with restless legs syndrome (RLS), also called Willis-Ekbom Disease. And while many turn to sleep aids or dopamine drugs, the real fix for a lot of people isn’t in a pill bottle at all-it’s in their iron levels.
Why Your Legs Won’t Stop Moving
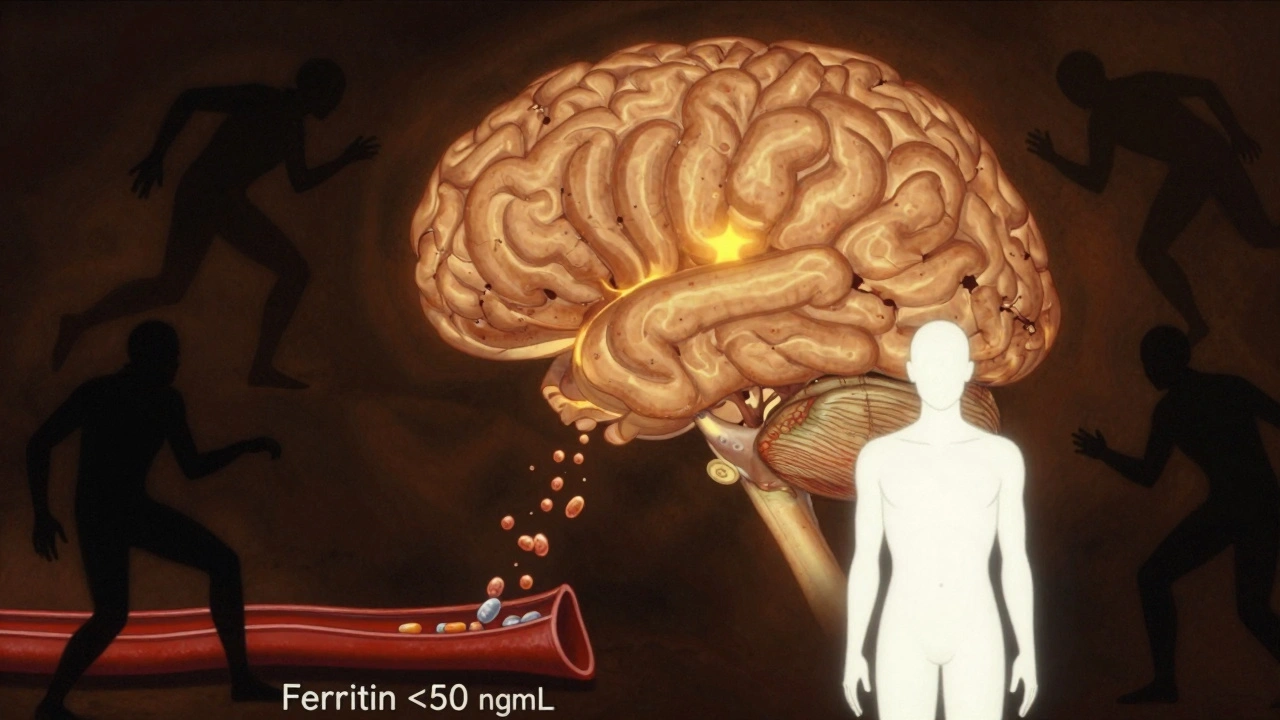
Restless legs syndrome isn’t just restlessness. It’s a neurological condition tied to how your brain uses iron. Even if your blood tests look normal, your brain might be starving for iron, especially in the area that controls movement and sensation. That’s why symptoms hit hardest at night, when you’re still and your brain has nothing else to focus on. The urge to move isn’t anxiety. It’s your nervous system screaming for balance.The Magic Number: Ferritin Below 50 ng/mL
Most doctors check ferritin-the protein that stores iron-and think you’re fine if it’s above 12 ng/mL. That’s the old lab range. But for RLS, that number is meaningless. Research from Johns Hopkins, the American Academy of Neurology, and multiple sleep clinics shows the real cutoff is 50 ng/mL. If your ferritin is below that, you’re likely dealing with brain iron deficiency, even if your hemoglobin is normal. Studies show that people with ferritin under 50 have worse symptoms and are more likely to develop augmentation-a nasty side effect of dopamine drugs where RLS gets worse over time, spreads to other body parts, or starts earlier in the day. Fix the iron, and you might avoid those drugs entirely.Why Oral Iron Often Fails
You might’ve tried iron pills and felt nothing. That’s not your fault. Most people take ferrous sulfate-65 mg of elemental iron per tablet-and expect results in a week. But here’s the catch: your gut doesn’t absorb it well, especially if you have inflammation, gut issues, or high levels of hepcidin (the hormone that blocks iron absorption). In fact, up to 30% of people can’t tolerate the stomach upset, and another 20% just don’t absorb enough to raise ferritin. A 2020 study in Blood Advances found that taking iron every other day-not daily-boosts absorption and cuts side effects. Why? Your body gets a chance to reset its iron sensors. You still get the same total dose, but your gut handles it better.What to Take and How
If your ferritin is under 50, start with:- 65 mg elemental iron per day (usually 325 mg ferrous sulfate)
- Take it on an empty stomach-at least 1 hour before or 2 hours after food
- Pair it with vitamin C-100-200 mg. Orange juice or a supplement helps iron absorb 2-3x better
- Alternate days if you get nausea or constipation
When Oral Iron Isn’t Enough
If you’ve tried 3-4 months of oral iron and your ferritin is still under 30, or you can’t tolerate the pills, IV iron is the next step. It’s not scary-it’s a simple 15-30 minute infusion. Ferric carboxymaltose (brand name Injectafer) is the go-to for RLS. One dose of 1000 mg can raise ferritin by 127 ng/mL on average, and 68% of patients report major symptom relief within 6 weeks. A 2021 study in Sleep Medicine showed that after a single IV iron infusion, patients had better sleep, less leg movement, and fewer nighttime awakenings. And unlike dopamine drugs, IV iron doesn’t cause augmentation. The effects last up to 2 years.Cost and Long-Term Value
Oral iron costs about $10-$20 a month. IV iron runs $800-$1,200 per infusion-but it’s often covered by insurance for RLS patients with ferritin under 50. Compare that to pramipexole or ropinirole, which cost $200-$400 a month and come with risks of impulse control disorders, dizziness, and hallucinations. A 2022 analysis in the Journal of Medical Economics found that switching from dopamine drugs to iron therapy saves an average of $3,500 per patient per year. Not just in drug costs, but fewer doctor visits, less sleep aid use, and fewer missed workdays.What About Diet?
Eating more red meat or spinach won’t fix RLS if your ferritin is low. Heme iron from beef gives you about 1-2 mg per serving. You need 65 mg daily to make a difference. That’s like eating 30 steaks a day. Even if you could, your body still wouldn’t absorb it efficiently if hepcidin is high. Diet is supportive, not curative. Focus on getting enough vitamin C with meals, and avoid tea or coffee with iron-rich foods. But don’t rely on food alone.
Testing and Monitoring
Don’t just test ferritin once and call it done. Get these labs before starting iron:- Ferritin (target: ≥75 ng/mL for best symptom control)
- Serum iron
- Total iron-binding capacity (TIBC)
- Transferrin saturation
- Hepcidin (if available-still research-grade but promising)
Who Should Skip Iron?
Iron isn’t for everyone. Avoid it if you have:- Hemochromatosis (genetic iron overload)
- Active infection or inflammation
- Severe liver disease
- History of iron poisoning
What’s Next in RLS Treatment
New iron formulations are coming. Liposomal iron and ferric maltol are designed to be gentler on the stomach and absorb better. Early trials show 40% higher absorption and 60% fewer side effects than ferrous sulfate. These aren’t widely available yet, but they’re on the horizon. The American Academy of Sleep Medicine is expected to update its guidelines in 2024 to recommend IV iron as a first-line option for RLS patients with ferritin under 75 ng/mL. That’s a big shift-from treating symptoms to treating the root cause.Bottom Line
If you have restless legs and your ferritin is below 50 ng/mL, iron therapy isn’t just an option-it’s your best shot at long-term relief without the risks of dopamine drugs. Most people see improvement in 4-8 weeks. It’s not instant, but it’s sustainable. And unlike pills that make your symptoms worse over time, iron fixes the problem at the source. Start with a blood test. Don’t wait for your doctor to suggest it-ask for ferritin specifically. If it’s low, start iron. If it doesn’t help, dig deeper. You’re not just dealing with leg discomfort. You’re dealing with a brain that’s running on empty. And sometimes, all it needs is a little more iron to finally rest.Can low iron cause restless legs even if I’m not anemic?
Yes. Anemia means low hemoglobin, but restless legs syndrome is tied to brain iron deficiency, not blood iron. You can have normal hemoglobin and still have ferritin under 50 ng/mL-which is enough to trigger RLS symptoms. Many people with RLS are not anemic but still respond dramatically to iron therapy.
How long does it take for iron to work for restless legs?
Most people notice improvement in 4-8 weeks. Some feel better in 2-3 weeks, especially with IV iron. Oral iron takes longer because absorption is slow and inconsistent. Don’t give up before 8 weeks unless you have severe side effects.
Is IV iron safe for RLS?
Yes, when given under medical supervision. Ferric carboxymaltose is approved for RLS and has been used safely in over 10,000 patients. Side effects are rare and usually mild-like temporary dizziness or headache. Serious reactions are extremely uncommon. It’s much safer than long-term dopamine drugs, which carry risks of addiction, impulse control disorders, and worsening symptoms.
Can I take iron with my other medications?
Avoid taking iron with calcium supplements, antacids, thyroid meds, or antibiotics like tetracycline. Wait at least 2 hours between them. Vitamin C helps iron absorb better, so take it together. If you’re on dopamine drugs for RLS, don’t stop them without talking to your doctor-iron can be added alongside them initially.
What if iron doesn’t help my restless legs?
If ferritin is above 75 and symptoms persist, the cause might not be iron. Other possibilities include nerve damage, kidney disease, pregnancy, or medications like antidepressants that worsen RLS. A sleep specialist can help rule these out. You might need a sleep study or nerve conduction test. Iron fixes the most common cause-but not all causes.
Should I get my ferritin checked if I have occasional leg discomfort?
If the discomfort happens mostly at night, makes you want to move your legs, and improves with movement, it’s worth testing. RLS is often misdiagnosed as muscle cramps or poor circulation. A simple ferritin test can rule out or confirm iron deficiency as the cause. No need to wait until symptoms are severe-early intervention works better.

