When a patient takes a pill labeled as a generic version of a brand-name drug, they expect the same effect - same relief, same safety, same outcome. But what if that pill was made in a factory thousands of miles away, under inspection rules that are anything but consistent? For many clinicians, that’s not a hypothetical. It’s a daily reality.
What’s really in that pill?
Generic drugs aren’t copies. They’re legally required to have the same active ingredient, strength, dosage form, and route of administration as the original. That’s the law. But here’s the catch: the FDA doesn’t require generics to match the brand-name drug in how they’re made. Not the machinery. Not the factory conditions. Not even where the ingredients come from. A single generic pill might have its active ingredient made in a plant in Hyderabad, India, mixed with inactive fillers in a facility in Pennsylvania, coated in a lab in China, and packaged in a warehouse in New Jersey. Only one company’s name appears on the label. The rest? Invisible. This isn’t a flaw in the system. It’s how the system was designed - to cut costs, not to guarantee consistency. And when cost becomes the top priority, corners get cut. That’s when quality starts to slip.The data clinicians can’t ignore
In 2023, researchers at Ohio State University analyzed over 1.3 million adverse event reports from the FDA’s database. They didn’t just look at which drugs caused problems. They looked at where those drugs were made. The results were stark. Generic drugs manufactured in India were linked to a 54% higher rate of severe adverse events - including hospitalizations, permanent disability, and death - compared to identical generics made in the U.S. The difference wasn’t small. It was dramatic. And it got worse with older drugs. Why? Because as price pressure mounts, manufacturers in low-cost countries start cutting corners. They use cheaper raw materials. They skip maintenance on aging equipment. They rush production. And when you’re making a drug that sells for $0.10 a pill, there’s no profit margin left for quality control. Dr. Robert S. Gray, lead researcher on the study, put it bluntly: “As drugs get cheaper and cheaper and the competition gets more intense to hold down costs, you end up with operations and supply chain issues that can compromise drug quality.”The inspection gap
The FDA claims it inspects all facilities - domestic and foreign - to ensure safety. But here’s the truth: inspections in the U.S. are unannounced. You show up, and you check the facility. No warning. No time to clean up. In India and China? Inspections are scheduled weeks in advance. Companies know exactly when the inspectors are coming. They fix the broken machines. They hide the moldy batches. They clean the floors. They put on a show. Professor Gray calls this “a regulatory loophole that lets manufacturers hide problems.” And it’s not just about cleanliness. It’s about process control. A single batch of a generic blood thinner made in a facility without real-time monitoring can have inconsistent potency - enough to cause a stroke in one patient and do nothing in another. The FDA has over 1,300 staff focused on drug quality. But they’re inspecting over 4,000 foreign facilities. That’s one inspector for every three factories. And many of those facilities haven’t been inspected in years.
Why older generics are the most dangerous
Not all generics are created equal. The newer ones - those that came to market in the last decade - are often made with modern equipment and better quality systems. But the older ones? The ones doctors prescribe every day for high blood pressure, depression, or diabetes? Many were approved 20, 30, even 40 years ago. These older drugs were never meant to be made on outdated, 1970s-era machinery. But that’s exactly what’s happening. The companies that make them have no incentive to upgrade. Why spend $5 million on new technology when you can keep making the same drug for $0.05 a pill and still make a profit? Duke-Margolis Center researchers found that manufacturing quality issues are the leading cause of drug shortages - and the shortages are worst for these older, low-cost generics. When a batch fails inspection, there’s no backup. No alternative supplier. No quick fix. Patients go without. And when patients go without? Mortality rates rise. Cancer treatments get delayed. Heart patients miss doses. Emergency rooms fill up with people who had preventable complications.What’s being done - and what’s not
The FDA has started promoting advanced manufacturing technologies - things like continuous manufacturing and real-time quality monitoring. These systems can catch problems as they happen, not weeks later after a batch has already shipped. Over 80% of drugs made with these technologies are produced in the U.S. That’s not a coincidence. It’s because the cost of upgrading equipment is too high for manufacturers who rely on low-margin, outsourced production. Some experts suggest making manufacturing location transparent. Imagine if every generic drug label listed where the active ingredient was made. Not just the final packaging site - but the actual source. Patients could choose. Clinicians could track. Pharmacies could avoid high-risk suppliers. But the FDA hasn’t required it. And pharmaceutical distributors? They’re not pushing for it. Why? Because transparency means accountability. And accountability means higher costs.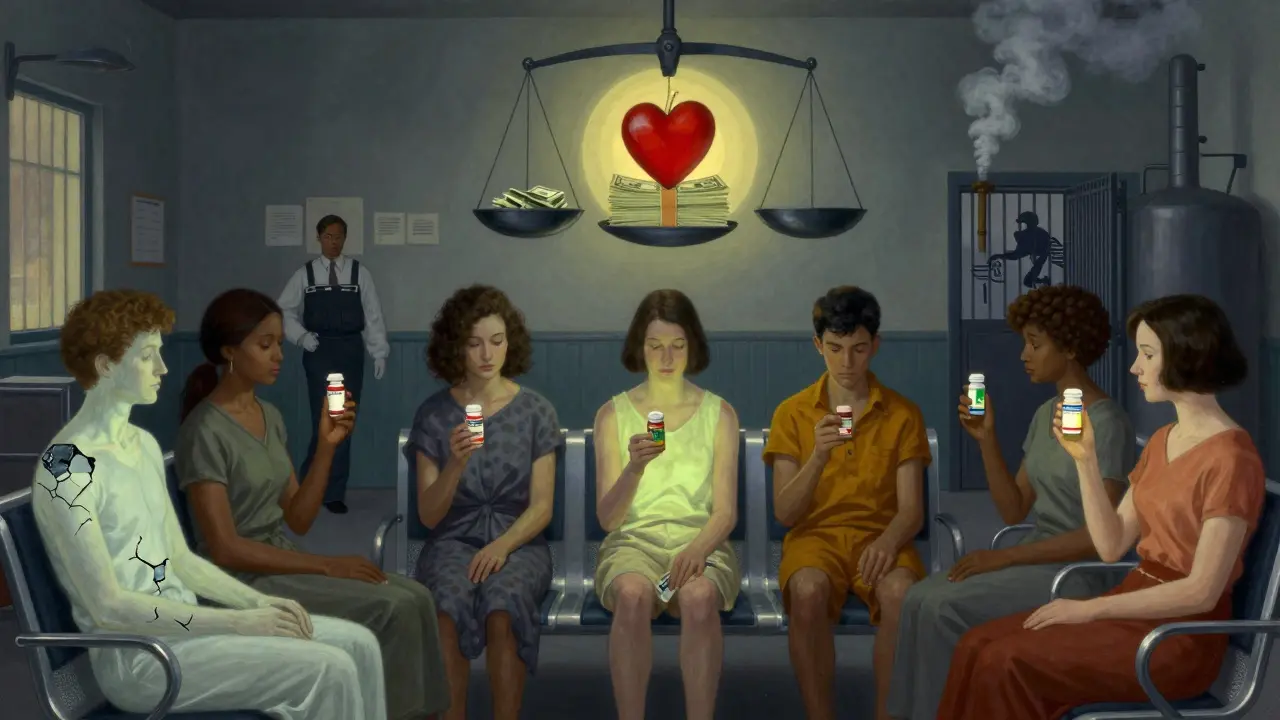
The domestic solution
The University of Wisconsin School of Pharmacy says it plainly: “If we have more generic manufacturing happening domestically, we would ideally have fewer quality concerns, fewer shortages, and a more resilient pharmaceutical supply chain.” It’s not about patriotism. It’s about control. When a drug is made in the U.S., you can walk into the facility. You can inspect it. You can shut it down if something’s wrong. You can’t do that from 8,000 miles away. Some manufacturers are starting to shift back. A few U.S. companies are investing in small-batch, high-quality generic production. They’re not trying to compete on price. They’re competing on trust. And clinicians? They’re noticing. More are asking pharmacists: “Where’s this made?”What clinicians can do
You don’t need to wait for policy changes to act. Here’s what you can do right now:- Ask your pharmacy: “Can you tell me where this generic drug was manufactured?” Many don’t know - but they should be able to find out.
- Track adverse events. If a patient has an unexpected reaction to a generic, document it. Report it to the FDA. Numbers matter.
- When multiple generics are available, choose the one with the most recent manufacturing date. Newer batches are more likely to come from better-controlled facilities.
- Support policies that fund domestic generic manufacturing. It’s not expensive in the long run - it’s cheaper than treating preventable hospitalizations.

