When you walk into a pharmacy to pick up your prescription, you might not realize you have the legal right to say no. Many patients assume the pharmacist will automatically swap their brand-name medication for a cheaper generic version - and in many cases, they do. But you don’t have to accept that switch. In fact, under U.S. law, you can refuse generic substitution and request your brand-name drug instead. This isn’t just a preference - it’s a protected right, and knowing how to exercise it can make a real difference in your health.
What Is Generic Substitution?
Generic substitution means a pharmacist replaces your prescribed brand-name drug with a chemically identical generic version. These generics contain the same active ingredient, dosage, and intended effect as the brand. The FDA requires them to meet strict standards for safety and effectiveness. For many drugs, this swap works perfectly - and saves you money. In fact, generic drugs cost, on average, 80-85% less than their brand-name counterparts. That’s why pharmacies and insurance companies push for substitution: it cuts costs across the system.But not all drugs are created equal. Some medications have a narrow therapeutic index (NTI), meaning even tiny changes in dosage or formulation can cause serious side effects or treatment failure. Examples include thyroid meds like levothyroxine, epilepsy drugs like phenytoin, and blood thinners like warfarin. For these, switching brands - even to a generic labeled as “therapeutically equivalent” - can throw your body off balance. Patients with diabetes, heart conditions, or autoimmune disorders often report unexpected changes in symptoms after an unplanned switch.
Your Legal Right to Say No
All 50 U.S. states and Washington, D.C. have laws about generic substitution, but they’re not the same. In 19 states - including California, Texas, and Florida - pharmacists are required to substitute unless the prescriber says otherwise. But in 7 states - Alaska, Connecticut, Hawaii, Maine, Massachusetts, New Hampshire, and Vermont - plus D.C., the law requires your explicit consent before any substitution happens. That means the pharmacist must ask you, “Do you want the generic?” and you can say no.Even in states where substitution is automatic, you still have the right to refuse. You don’t need a doctor’s note or a special form. Simply saying, “I decline substitution,” is legally enough in 43 states. Pharmacists can’t pressure you, claim it’s mandatory, or imply you’ll pay more if you refuse. If they do, they’re violating state law.
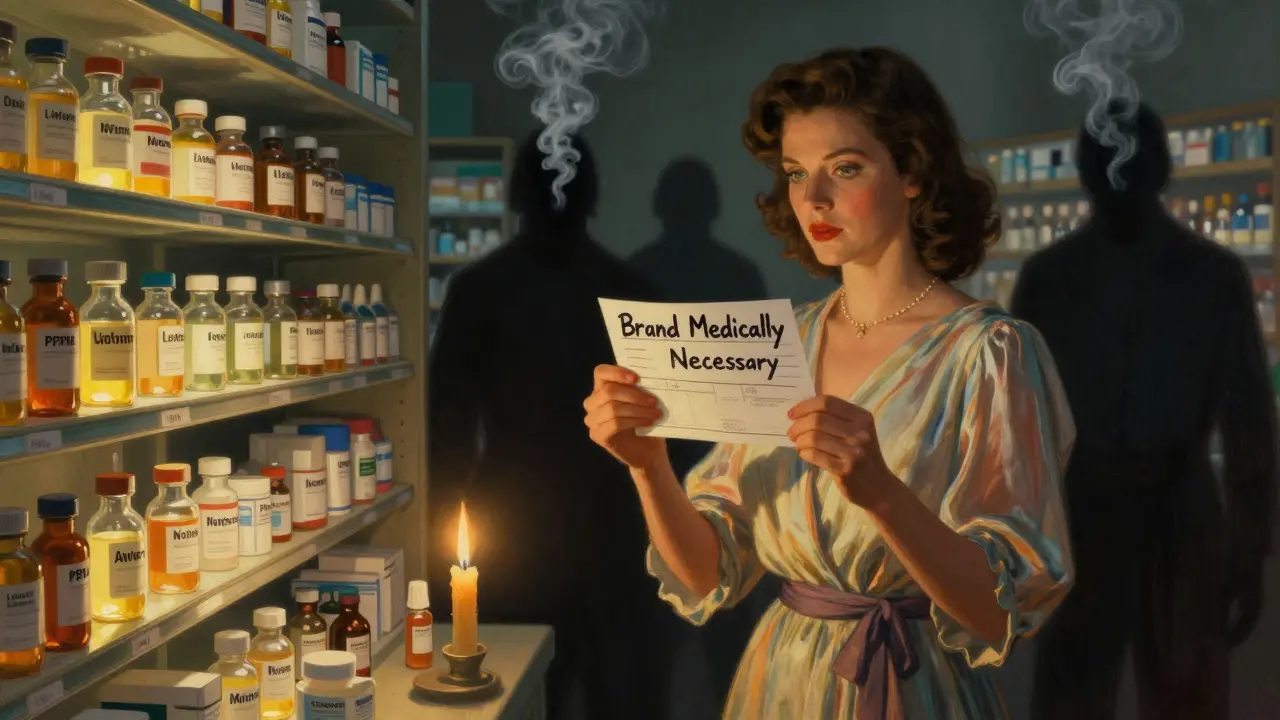
When Brand-Name Drugs Are Medically Necessary
If your doctor believes you need the brand-name version - whether because of past reactions, NTI concerns, or stability issues - they can write “Dispense as Written” or “Brand Medically Necessary” on your prescription. Forty-eight states recognize this notation as a legal barrier to substitution. You don’t need to explain why; the law respects the prescriber’s judgment.For biologics - complex drugs like insulin, Humira, or Enbrel - the rules are even stricter. All 50 states allow prescribers to block substitution, and 47 states now require pharmacists to notify your doctor if they switch you to a biosimilar. That’s because biosimilars aren’t exact copies like traditional generics - they’re highly similar but not identical. Some patients report erratic blood sugar levels or immune reactions after an unsanctioned switch.
What to Do at the Pharmacy
Here’s how to protect your rights when picking up your prescription:- Speak up before payment: Say clearly, “I’m refusing generic substitution,” or “I need the brand-name drug.” Don’t wait until after they’ve already filled the prescription.
- Ask for the manager: If the pharmacist argues, insists they “have to” substitute, or claims you’ll pay more, ask to speak with the pharmacy manager. They’re trained on state laws and should know the rules.
- Know your state’s law: If you live in a state that requires consent (like Massachusetts or Hawaii), you can cite it. Example: “In my state, the law says I must give consent before a substitution.”
- Get a written note from your doctor: If you have a chronic condition or have had bad reactions before, ask your provider to write “Brand Medically Necessary” on all future prescriptions.
- Keep records: Note the date, drug name, and what happened. If you’re denied your requested drug, file a complaint with your state’s Board of Pharmacy.
Why Some Pharmacies Push Substitution
Pharmacies aren’t trying to harm you. They’re caught in a system designed to cut costs. Pharmacy Benefit Managers (PBMs) like CVS Caremark and Express Scripts control which drugs get covered and at what price. They often push generics because they get rebates from manufacturers. In some cases, they even used to hide the fact that paying cash for the brand-name drug might be cheaper than using insurance - a practice called a “gag clause.” That was banned nationwide in 2018 by the Know the Lowest Price Act.Now, pharmacists can legally tell you: “The brand costs less than your co-pay.” If you’re paying out of pocket, ask. You might save money - and avoid a risky switch.
Real Patient Stories
One patient in Massachusetts refused substitution for Synthroid after her TSH levels spiked following a generic switch. She told the pharmacist, “I decline substitution per state law,” and got her brand-name drug without paying more. Her doctor later confirmed the change was likely responsible for her symptoms.In contrast, a diabetic patient in Texas was switched from Lantus to Basaglar without notice. Her blood sugar became erratic for weeks before she figured out what had changed. She filed a complaint with her state’s pharmacy board - and got a refund.
These aren’t rare cases. A 2021 Consumer Reports survey found 28% of patients who tried to refuse substitution faced resistance. But 83% of those who were properly informed about their rights said they were satisfied with the outcome.

What to Do If You’re Denied
If a pharmacy refuses your request - especially in a state that requires consent - take action:- Ask for a written explanation of why they denied your request.
- Contact your state’s Board of Pharmacy. All 50 states have a complaint process - often online and free.
- Report the incident to the FDA’s MedWatch program if you experienced a side effect.
- Inform your doctor. They may need to update your prescription or file an appeal with your insurer.
Pharmacies can be fined for violating substitution laws. In 2019, a Michigan pharmacy was sued after a patient suffered seizures following an unauthorized switch of an antiepileptic drug. The case set a precedent: pharmacists can be held liable when they ignore patient rights.
Bottom Line: You’re Not Just a Number
Generic substitution saves billions - but not at the cost of your health. You have the right to choose what goes into your body. Whether you’re on thyroid medication, insulin, or an antiseizure drug, your voice matters. Don’t let confusion or pressure take that choice away. Know your state’s rules. Speak up. Keep records. And if you’re told you can’t refuse - you’re being lied to.Can I refuse a generic drug even if my insurance covers it?
Yes. Insurance coverage doesn’t override your right to refuse substitution. Even if your plan prefers generics, you can still ask for the brand-name drug. In some cases, you may pay more out of pocket - but not always. Sometimes, the brand-name drug costs less than your co-pay, especially after the 2018 ban on gag clauses. Always ask the pharmacist to compare cash price versus insurance cost.
Do I need a doctor’s note to refuse substitution?
No, not always. In 43 states, simply saying “I decline substitution” is legally sufficient. However, if you have a medical reason - like past adverse reactions or a narrow therapeutic index drug - a doctor’s note saying “Brand Medically Necessary” makes your request stronger and prevents future issues. Some states require this notation to block substitution entirely.
What if the pharmacist says they’re required to substitute?
That’s false in states requiring consent. In Alaska, Connecticut, Hawaii, Maine, Massachusetts, New Hampshire, Vermont, and D.C., pharmacists must get your permission before substituting. In other states, substitution may be automatic - but you still have the right to refuse. If they claim it’s mandatory, ask to speak with the manager and cite your state’s pharmacy law. You can also call your state’s Board of Pharmacy for confirmation.
Are biosimilars the same as generics?
No. Biosimilars are not exact copies like traditional generics. They’re highly similar versions of complex biologic drugs - like insulin or rheumatoid arthritis treatments - but made from living cells. Because they’re more complex, small differences can affect how they work. That’s why 47 states now require pharmacists to notify your doctor before switching you to a biosimilar. Always ask if what you’re getting is a biosimilar, not a generic.
Can I get my brand-name drug if it’s not on my insurance formulary?
Yes, but you’ll likely pay more. If your drug isn’t covered, you can still request it and pay cash - or ask your doctor to file a prior authorization with your insurer. Some insurers approve brand-name drugs for medical necessity, especially for NTI drugs or patients with prior adverse reactions. Keep documentation of any side effects or lab results that support your case.

