Most people don’t feel high cholesterol. No pain. No warning. No symptoms. That’s why it’s so dangerous. By the time you notice something’s wrong-chest pain, shortness of breath, a heart attack-it’s often too late. High cholesterol, or hypercholesterolemia, isn’t just a number on a lab report. It’s a silent threat building up inside your arteries, year after year, until something breaks.
What Exactly Is Hypercholesterolemia?
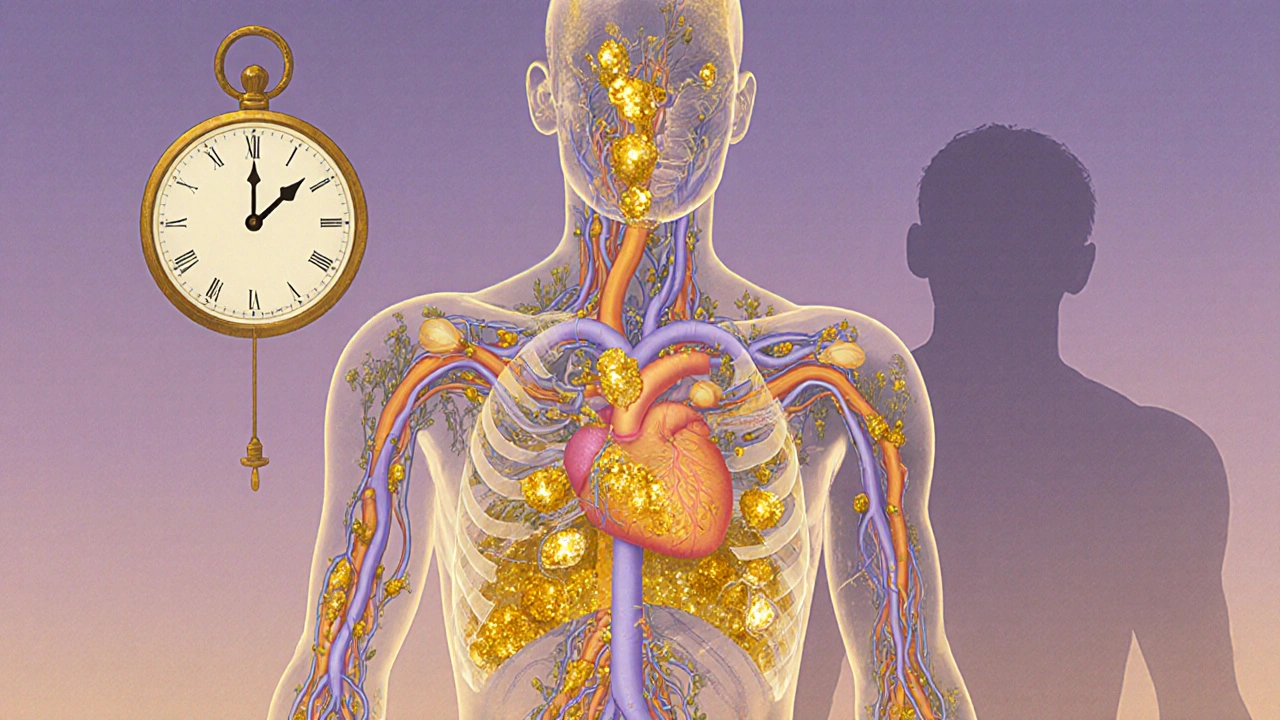
Hypercholesterolemia means your blood has too much cholesterol-specifically, too much of the bad kind: low-density lipoprotein, or LDL. Cholesterol isn’t all bad. Your body needs it to make hormones, digest food, and build cells. But when LDL levels climb too high, it sticks to artery walls, forming plaques. Over time, those plaques narrow your blood vessels. That’s atherosclerosis. And that’s what leads to heart attacks and strokes.
The numbers matter. According to the American Heart Association, more than 93 million American adults have total cholesterol above 200 mg/dL. But it’s not just about the total. LDL is the real villain. Levels above 190 mg/dL are considered severe. Even between 130 and 159 mg/dL, if you have other risk factors like high blood pressure or diabetes, your risk goes up fast.
There are two main types. One is genetic-familial hypercholesterolemia (FH). The other is lifestyle-driven. FH isn’t rare. It affects about 1 in 250 people worldwide. People with FH are born with defective genes that stop their bodies from clearing LDL properly. Some have LDL levels over 450 mg/dL by age 10. Without treatment, men with FH often have heart attacks before 50. Women before 60.
How Do You Know If You Have It?
You can’t feel it. You can’t see it. The only way to know is a simple blood test. The good news? You don’t need to fast anymore. Most lipid panels today work just fine without fasting. The U.S. Preventive Services Task Force recommends testing everyone between 40 and 75. But if you have a family history of early heart disease, or if you’re overweight, diabetic, or smoke, get tested sooner-even in your 20s or 30s.
Some physical signs can hint at FH. Yellowish fatty deposits around the eyelids (xanthelasmas). Thickened tendons, especially in the heels or knuckles (tendon xanthomas). These aren’t common in everyday high cholesterol, but if you see them, it’s a red flag. A doctor should check for FH right away.
Familial vs. Lifestyle-Driven High Cholesterol
Not all high cholesterol is the same. Familial hypercholesterolemia is like a genetic time bomb. Even if you eat perfectly, exercise daily, and never smoke, your LDL can still be sky-high. That’s because your body can’t remove it. Lifestyle changes alone won’t cut it. Most people with FH need medication from day one-often a combo of statins, ezetimibe, and newer drugs like PCSK9 inhibitors.
On the other hand, most people with high cholesterol have it because of what they eat, how much they move, or other health conditions. Eating too much saturated fat (think fried foods, fatty meats, butter) raises LDL. Being overweight, especially with belly fat, makes it worse. Diabetes and hypothyroidism are big contributors too. The good news? For these cases, diet and exercise can make a real difference.
The Portfolio Diet, studied in JAMA Cardiology, showed that swapping out saturated fats for oats, nuts, soy, and plant sterols can lower LDL by 10-15%-without drugs. That’s like taking a low-dose statin. But sticking to it? Hard. Only about half of people keep it up past a year.

What Happens If You Don’t Treat It?
Untreated hypercholesterolemia doesn’t just raise your risk of heart disease. It cuts your life short. The European Atherosclerosis Society says untreated heterozygous FH can shorten life by about 30 years. That’s not a guess. That’s based on decades of tracking real patients.
And it’s not just about the heart. Plaques in your neck arteries can cause strokes. Plaques in your legs can lead to pain when walking, or even amputation. Your kidneys, your brain, your whole body depends on clean, open blood vessels.
Here’s the scary part: most people don’t realize how high their cholesterol is until they’re already in the hospital. Dr. Roger Blumenthal from Johns Hopkins says cholesterol is a silent killer because symptoms don’t show until arteries are 70% blocked. By then, damage is done.
Treatment: It’s Not Just About Statins
Statins are the first line of defense. Drugs like atorvastatin and rosuvastatin can drop LDL by 50% or more. They’re cheap, well-studied, and proven to save lives. But they don’t work for everyone. About 7-29% of people can’t tolerate them-muscle pain, liver issues, or just can’t stick with them.
That’s where alternatives come in. Ezetimibe blocks cholesterol absorption in the gut. It’s not as strong as statins, but it adds about 18% more LDL reduction when combined with them. Then there are the PCSK9 inhibitors-alirocumab and evolocumab. These are injectables, given every two weeks or monthly. They can knock off another 50-60% of LDL on top of statins. They’re expensive, but for people with FH or very high risk, they’re life-changing.
And now there’s inclisiran (Leqvio). Approved in 2021, it’s a shot you get only twice a year. It works by silencing a gene that makes PCSK9, so your body clears LDL naturally. It’s a breakthrough for people who struggle with daily pills or frequent injections.
For FH patients, triple therapy is often needed: a high-intensity statin + ezetimibe + a PCSK9 inhibitor. It sounds intense, but for them, it’s the difference between a heart attack at 45 and living to 80.

Why So Many People Still Don’t Get Treated
Here’s the broken part: even though we have great tools, most people with high cholesterol aren’t getting the care they need. In the U.S., only about 55% of eligible adults are on statins. For Black adults, it’s 42%. For women, it’s 49%. In England, only half of high-risk patients hit their LDL targets.
Why? Cost. Side effects. Fear. Misinformation. Some think if they eat clean, they don’t need meds. Others think statins are dangerous. The truth? The risk of a heart attack from untreated high cholesterol is far greater than the risk of side effects from statins.
And adherence is terrible. Half of people stop taking their statin within a year. That’s not laziness. It’s often because doctors don’t follow up. Patients don’t understand why they need it. No one talks about the long-term payoff.
What You Can Do Right Now
If you’ve never been tested-get tested. It’s quick. It’s cheap. It could save your life.
If your LDL is high, don’t panic. But don’t wait. Talk to your doctor. Ask: What’s my number? What’s my goal? Do I need meds? What’s my plan?
Start with diet. Cut back on fried foods, fatty meats, and processed snacks. Swap butter for olive oil. Add oats, beans, nuts, and avocado. Eat more plants. You don’t need to be perfect. Just better.
Movement matters too. Just 30 minutes of brisk walking five days a week can lower LDL by 5-10%. You don’t need to run a marathon. Just move.
If you smoke-quit. Smoking damages your arteries. It makes cholesterol stickier. Quitting cuts your heart attack risk in half within a year.
And if you have a family history of early heart disease-tell your doctor. Even if you’re young. Even if you feel fine. Genetic testing for FH is available. Early diagnosis means early protection.
The Big Picture: Cholesterol Isn’t Just a Personal Problem
High cholesterol costs the U.S. $218 billion a year-$142 billion in medical bills, $76 billion in lost work. That’s not just about healthcare. It’s about families losing parents too soon. It’s about kids growing up without their mothers or fathers.
But there’s hope. The American Heart Association’s 2030 goal is to improve cardiovascular health by 20%. That means better diets, better access to meds, better follow-up care. New tools like inclisiran and polygenic risk scores are making it possible to predict and prevent high cholesterol before it becomes a crisis.
It’s not about being perfect. It’s about being aware. About taking one step. Then another. Because high cholesterol doesn’t have to be a death sentence. It just needs to be seen. And treated.