Medication Safety Checker for Older Adults
Check if your medications are potentially inappropriate for older adults based on the Beers Criteria. Enter the medications you're taking and learn about potential risks.
Add Your Medications
Enter all medications you're currently taking, including prescriptions, over-the-counter drugs, and supplements.
Medication #1
When you’re younger, a pill might just help you feel better. But as you get older, that same pill can make you dizzy, confused, or even send you to the hospital. It’s not because you’re being overly sensitive-it’s because your body is changing. And those changes affect how every medication you take works, how long it stays in your system, and how likely it is to cause harm.
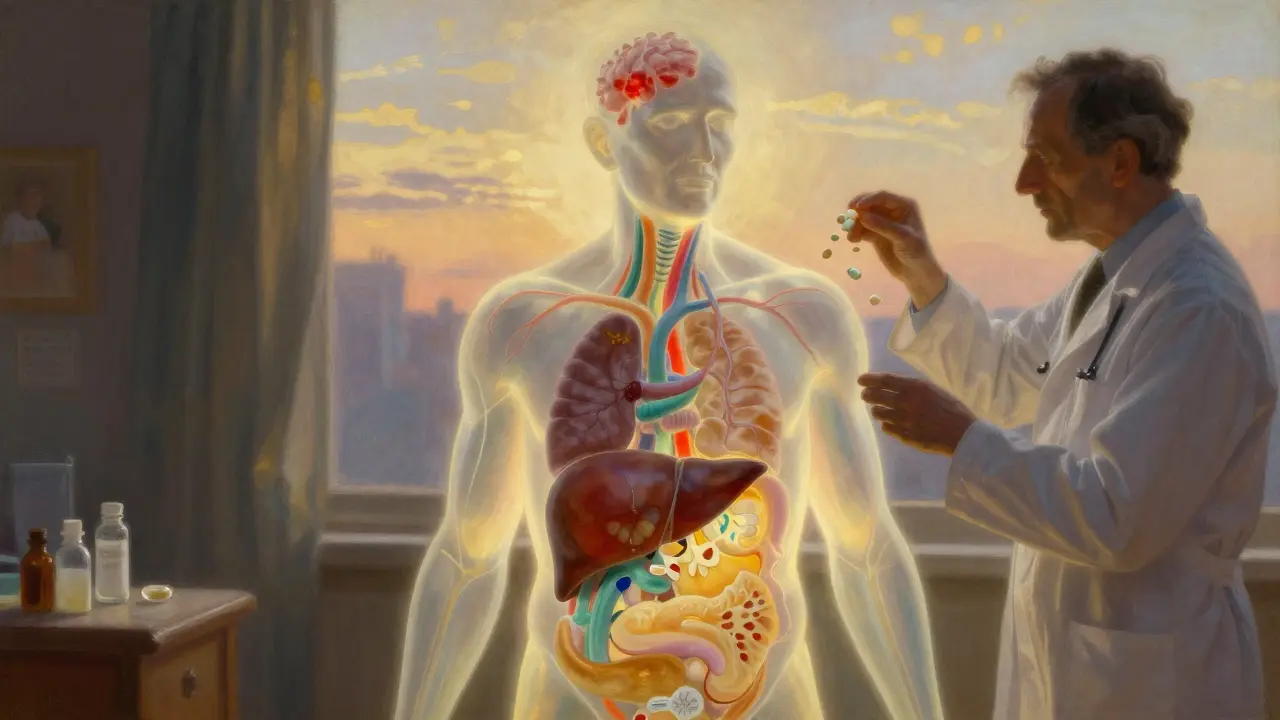
Why Older Bodies Handle Drugs Differently
Your body doesn’t stop changing when you turn 65. In fact, the way it processes medicine starts shifting decades before that. By the time you’re in your 70s or 80s, your kidneys, liver, and fat distribution have changed enough to turn a safe dose into a dangerous one.Take kidney function. After age 40, your kidneys slowly lose the ability to filter drugs out of your blood. On average, your glomerular filtration rate drops by about 0.8 mL/min/1.73m² every year. That means drugs like digoxin, antibiotics, or painkillers stick around longer. They build up. And instead of helping, they start causing problems-like confusion, irregular heartbeat, or even kidney damage.
Your liver isn’t working as hard either. Blood flow to the liver drops by 20-40% between ages 25 and 65. That affects how drugs like propranolol or verapamil are broken down. If your liver can’t process them fast enough, the drug stays in your system too long, increasing side effects.
Then there’s body composition. Between ages 25 and 80, total body water drops by 15%, while body fat increases. Water-soluble drugs like lithium or certain diuretics become more concentrated because there’s less water to dilute them. Fat-soluble drugs like diazepam or fluoxetine linger in fat tissue and release slowly, leading to prolonged effects-even if you took the same dose you did at 30.
Even your proteins change. Albumin, the main carrier for many drugs in your blood, declines by 10-15% in older adults. That means more of the drug is floating around unbound and active. For drugs like warfarin, this can mean your blood thins too much, raising your risk of dangerous bleeding-even if your lab numbers look fine.
How Your Brain and Heart React Differently
It’s not just about what your body does to the drug. It’s also about what the drug does to your body. As you age, your brain becomes more sensitive to certain medications.Take benzodiazepines. A dose of lorazepam or zolpidem that helps a 40-year-old sleep can leave an 80-year-old groggy, disoriented, and at risk of falling. Studies show older adults experience 2-3 times more falls and hip fractures from these drugs. One study found zolpidem caused 80% more next-day impairment in people over 65 compared to younger adults.
Anticholinergic drugs-common in allergy meds, sleep aids, and even some bladder treatments-can cause severe confusion or even delirium in older adults. A 2023 University of Florida study showed patients over 75 had 4.2 times higher rates of delirium than younger people taking the same dose. One Reddit user, age 78, described how amitriptyline for nerve pain led to urinary retention so bad he needed a catheter within three days.
Your heart responds differently too. Beta-blockers like propranolol require nearly 50% higher doses in younger people to achieve the same effect. In older adults, the heart doesn’t respond as strongly, so doctors sometimes increase the dose unnecessarily-only to find the patient’s blood pressure plummets when standing up. That’s orthostatic hypotension. A 2022 JAMA study found 28% of adults over 80 had symptoms from it, compared to just 9% of those aged 50-65.
The Polypharmacy Problem
Most older adults aren’t taking just one medication. The CDC reports that 48% of people over 65 take five or more prescription drugs every month. That’s called polypharmacy. And the more pills you take, the higher the chance they’ll interact-or that one of them will cause a side effect you didn’t expect.Take a typical scenario: Someone takes a blood pressure pill, a statin for cholesterol, a sleep aid, an antidepressant, and a painkiller. Each one affects the liver, kidneys, or brain. Together, they can cause dizziness, memory loss, constipation, or low sodium levels. One study found that 68% of older adults reported dizziness or falls linked to their meds. Another 54% said they felt confused or had memory problems.
And here’s the scary part: 35% of hospital admissions in people over 65 are due to medication side effects. Half of those could have been avoided.
The Beers Criteria and What Doctors Should Avoid
In 1991, the American Geriatrics Society created the Beers Criteria-a list of medications that are risky for older adults. It’s updated every two years. The 2023 version lists 56 drugs that should be avoided or used with extreme caution.Some of the most dangerous include:
- Diphenhydramine (Benadryl): A common OTC sleep aid that causes confusion and urinary retention.
- Nonsteroidal anti-inflammatories (NSAIDs) like ibuprofen: Increase risk of stomach bleeding and kidney failure.
- Benzodiazepines: High risk of falls and cognitive decline.
- Anticholinergics like oxybutynin: Linked to dementia and delirium.
- First-generation antihistamines: Cause drowsiness and low blood pressure.
These aren’t just warnings-they’re red flags. Yet a 2019 study found that 42% of older adults were still taking at least one of these drugs. And 15% had already suffered an adverse event because of them.
What Can Be Done? Practical Steps for Safer Medication Use
The good news? Many of these risks can be reduced. You don’t have to accept dizziness, confusion, or falls as part of aging.Start low, go slow. Doctors should begin with 25-50% of the standard adult dose for older patients, especially for drugs cleared by the kidneys. That’s not a suggestion-it’s standard practice.
Do a Brown Bag Review. Bring all your medications-prescription, over-the-counter, vitamins, supplements-to your doctor. A 2022 JAMA study found patients averaged 3.2 medication errors per visit. That includes duplicates, interactions, or drugs that are no longer needed.
Ask about deprescribing. Just because you started a drug years ago doesn’t mean you still need it. A 2023 study showed that 30-50% of medications in nursing homes are inappropriate. Ask your doctor: “Is this still helping me? Could I stop it safely?”
Check your kidney function. Don’t rely on creatinine alone. Ask for your eGFR (estimated glomerular filtration rate). If it’s below 60, your doses need adjusting.
Use the Beers Criteria app. It’s free, available on phones, and used by over 125,000 clinicians. You can even search your own meds to see if they’re flagged for older adults.
Real Stories, Real Risks
Behind every statistic is a person. One woman, 82, was prescribed the same blood pressure dose her doctor used for 50-year-olds. She fell, broke her hip, and spent months in rehab. Her story was posted on AgingCare.com. Another man stopped taking his antidepressant because it made him so constipated he couldn’t go to the bathroom. He didn’t tell his doctor-he just quit.These aren’t rare. A Merck Manuals survey found 45% of older adults stop taking their meds because of side effects. The top reasons? Constipation (28%), dizziness (24%), and confusion (19%).
What’s Changing in 2026
The system is slowly adapting. The FDA now encourages including patients over 75 in clinical trials. In 2023, 37 new age-adjusted medications were approved-the most in five years. Pharmacist-led medication reviews are now standard in 78% of U.S. hospitals. And AI tools like MedAware are reducing errors by 42%.But the biggest shift is cultural. Doctors are learning to ask not just “What should we add?” but “What can we stop?” The American Geriatrics Society is pushing for universal medication reviews for all Medicare beneficiaries by 2026.
And research is getting personal. Pharmacogenomics-testing your genes to see how you metabolize drugs-is showing real results. A 2023 study found testing for CYP2D6 and CYP2C19 genes reduced adverse reactions by 35% in older adults on antidepressants or antipsychotics.
Women over 65 experience 30% more side effects than men. Why? Differences in body fat, liver enzymes, and kidney function. This isn’t just a gender gap-it’s a dosing gap.
What You Can Do Today
You don’t need to wait for the system to fix itself. Here’s what you can do right now:- Make a list of every pill, patch, and supplement you take. Include doses and why you take them.
- Ask your doctor: “Could any of these be causing my dizziness or confusion?”
- Ask: “Is there a safer alternative?”
- Ask: “Can I stop any of these?”
- Bring your list to every appointment-even if it’s for a cold.
Medication isn’t the enemy. But treating older adults like younger ones is. Your body changes. Your meds should too.
Why do older adults have more side effects from medications?
Older adults have more side effects because their bodies process drugs differently. Kidneys and liver slow down, body fat increases, and protein levels drop. This means drugs stay in the system longer, build up to toxic levels, or become more active. The brain and heart also become more sensitive-so even normal doses can cause dizziness, confusion, or falls.
What is the Beers Criteria?
The Beers Criteria is a list of medications that are potentially inappropriate for older adults because they carry a high risk of side effects. Updated every two years by the American Geriatrics Society, it identifies 56 drugs to avoid or use with caution, including benzodiazepines, anticholinergics, and NSAIDs. It’s used by doctors and pharmacists to guide safer prescribing.
What is polypharmacy, and why is it dangerous for older adults?
Polypharmacy means taking five or more medications at once. It’s common in older adults, with nearly half of those over 65 doing so. The danger is that each drug can interact with others, increasing side effects like confusion, falls, kidney damage, or bleeding. The more pills you take, the harder it is to know which one is causing a problem.
Can older adults stop taking some of their medications safely?
Yes, and often they should. Many medications prescribed years ago may no longer be needed-or may be doing more harm than good. This process is called deprescribing. Studies show 30-50% of medications in nursing homes are inappropriate. Stopping them under medical supervision can improve energy, reduce falls, and even improve memory.
What should I bring to my doctor’s appointment about my medications?
Bring everything you take: prescription pills, over-the-counter drugs, vitamins, herbs, and supplements. Include the name, dose, and why you take it. This is called a Brown Bag Review. It helps your doctor spot duplicates, interactions, or drugs that are no longer useful. On average, patients have 3.2 medication errors per review.
Are there tools to help me check if my meds are safe for older adults?
Yes. The Beers Criteria app is free and available on smartphones. It lets you search your medications to see if they’re flagged as risky for older adults. Many hospitals and pharmacies also use digital tools like MedAware that flag potential errors before prescriptions are filled.