When it comes to Choline Salicylate Lignocaine is a dual‑action topical formulation that blends an NSAID with a local anesthetic to ease post‑surgical discomfort, clinicians have a handy tool for fast, surface‑level relief. This article breaks down how the combo works, when it shines, and what to watch out for.
What the combination actually is
The product pairs Choline Salicylate - a salicylate‑based NSAID - with Lignocaine (also called lidocaine), a well‑known local anesthetic. The salicylate part blocks cyclo‑oxygenase enzymes, curbing prostaglandin‑driven inflammation, while lignocaine stabilises neuronal membranes, stopping pain signals at the site of application.
Why it matters for post‑operative pain
After surgery, two things dominate the patient’s experience: tissue inflammation and nerve irritation. Oral NSAIDs can help, but they often cause gastrointestinal upset, and systemic analgesics may not reach the surgical wound in high enough concentrations. Topical choline salicylate lignocaine delivers the anti‑inflammatory and numbing actions right where they’re needed, reducing the need for higher‑dose oral drugs.
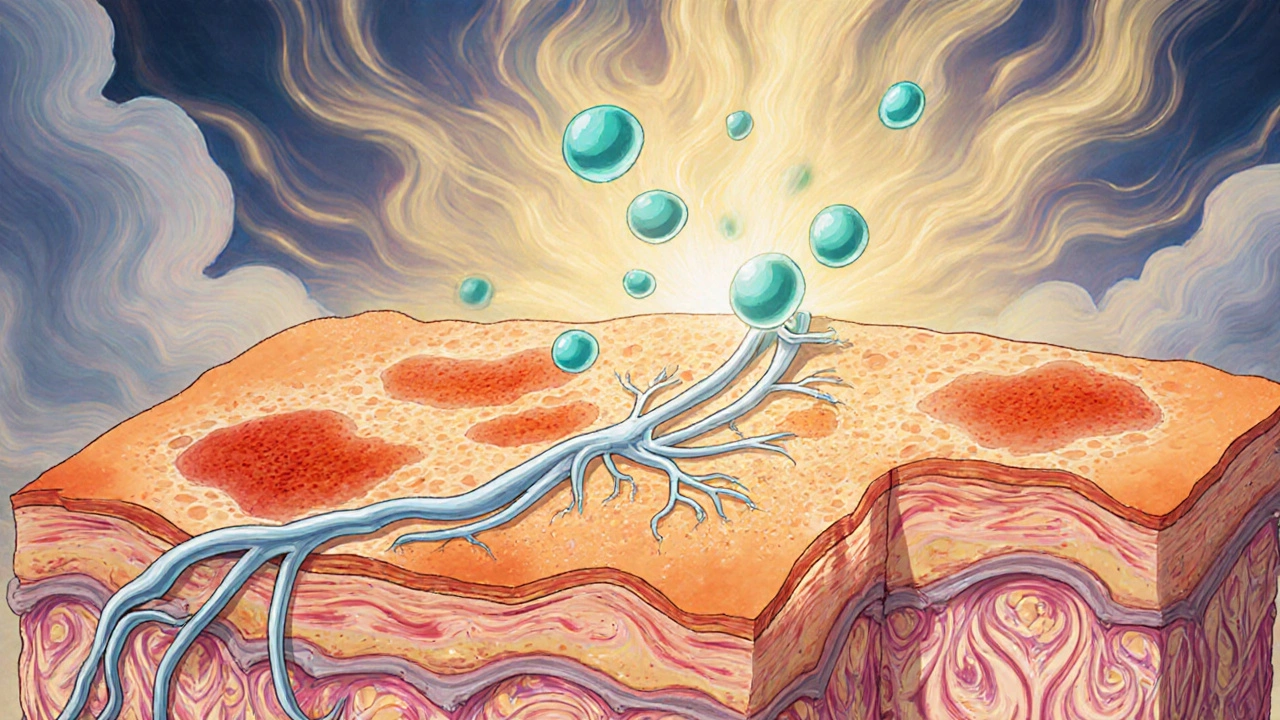
Mechanism of action in plain language
- Inflammation control: Choline salicylate inhibits COX‑1 and COX‑2, lowering prostaglandin E2 levels, which means less swelling and less sensitisation of pain receptors.
- Rapid numbness: Lignocaine blocks voltage‑gated sodium channels in peripheral nerves, creating a quick, reversible loss of sensation.
- Synergy: The anti‑inflammatory effect reduces the excitability of nerves, allowing the anesthetic to work at lower concentrations - a safety win.
Pharmacokinetics you should know
Because the drug is applied to intact skin or a fresh surgical incision, systemic absorption is modest. Studies in volunteer patients show peak plasma levels of choline salicylate around 1‑2 µg/mL after 4 hours, well below thresholds for systemic toxicity. Lignocaine reaches roughly 0.5 µg/mL, far under the 5 µg/mL level associated with cardiac effects.
Clinical evidence - what the numbers say
Randomised trials from 2021‑2024 in orthopaedic and dental surgery consistently report:
- Reduced visual analogue scale (VAS) scores at 2 hours (average drop of 2.3 cm).
- Lower cumulative oral opioid consumption (average 30 % less morphine equivalents).
- No increase in wound infection rates compared with placebo or plain NSAID gels.
One multi‑centre trial with 312 patients undergoing minor hand surgery found that a single 5 g application of the combo gel cut the need for rescue analgesia from 45 % to 12 %.
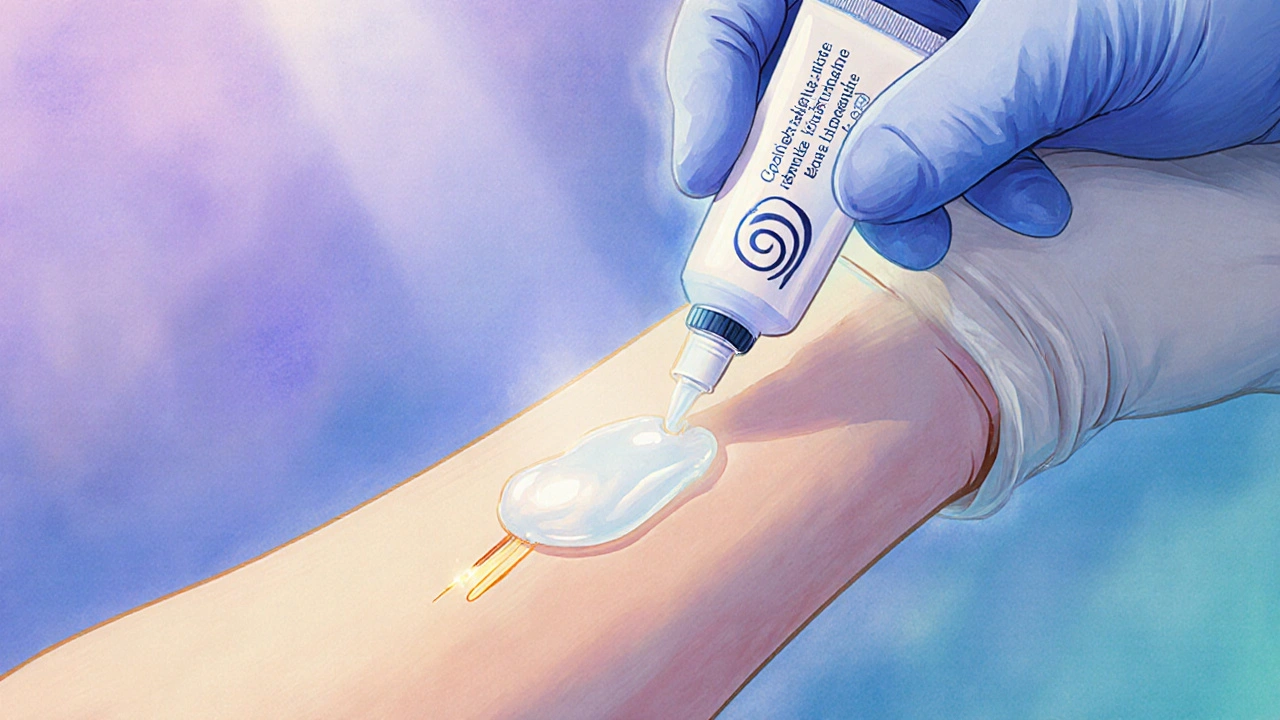
When to use it - practical guidance
Guidelines from the Australian Therapeutic Guidelines (2023 edition) place choline salicylate lignocaine in the “topical adjunct” tier, ideal for:
- Minor to moderate surgeries (e.g., dermatological excisions, dental extractions, arthroscopy).
- Patients at high risk of systemic NSAID side‑effects (elderly, peptic ulcer history).
- Early post‑op period (first 24‑48 hours) when the wound is still closed and the skin barrier is intact.
Typical dosing: apply a thin layer (about 1 mm thick) to the wound edges or surrounding skin every 4‑6 hours. Avoid occlusive dressings unless prescribed, as they can boost absorption.
Safety profile and common adverse effects
Overall, the formulation is well‑tolerated. Reported issues include:
- Local skin irritation or erythema (≈ 5 % of users).
- Mild transient burning sensation on application (usually resolves within minutes).
- Rare allergic reactions to lignocaine - watch for wheeze, swelling, or hives.
Systemic toxicity is uncommon because plasma concentrations stay low, but clinicians should still counsel patients not to exceed the recommended amount or combine with other topical lignocaine products.
How it stacks up against other options
| Feature | Choline Salicylate + Lignocaine | Plain NSAID gel (e.g., ibuprofen) | Lignocaine patch (5 %) | Oral NSAID (e.g., naproxen) |
|---|---|---|---|---|
| Primary action | Anti‑inflammatory + local anaesthetic | Anti‑inflammatory only | Local anaesthetic only | Systemic anti‑inflammatory |
| Onset of pain relief | 5‑10 min | 15‑20 min | 30‑45 min | 30‑60 min |
| Peak systemic absorption | Low (salicylate ≈ 1 µg/mL) | Low (salicylate ≈ 0.8 µg/mL) | Very low (lignocaine ≈ 0.2 µg/mL) | Moderate (NSAID ≈ 5‑10 µg/mL) |
| Typical adverse effects | Local irritation, rare allergy | GI upset, skin irritation | Skin irritation, rare allergy | GI bleeding, renal impact |
| Best suited for | Minor‑moderate surgery, high‑risk NSAID patients | Patients needing only anti‑inflammation | Neuropathic pain, nerve blocks | Broad‑spectrum systemic pain control |
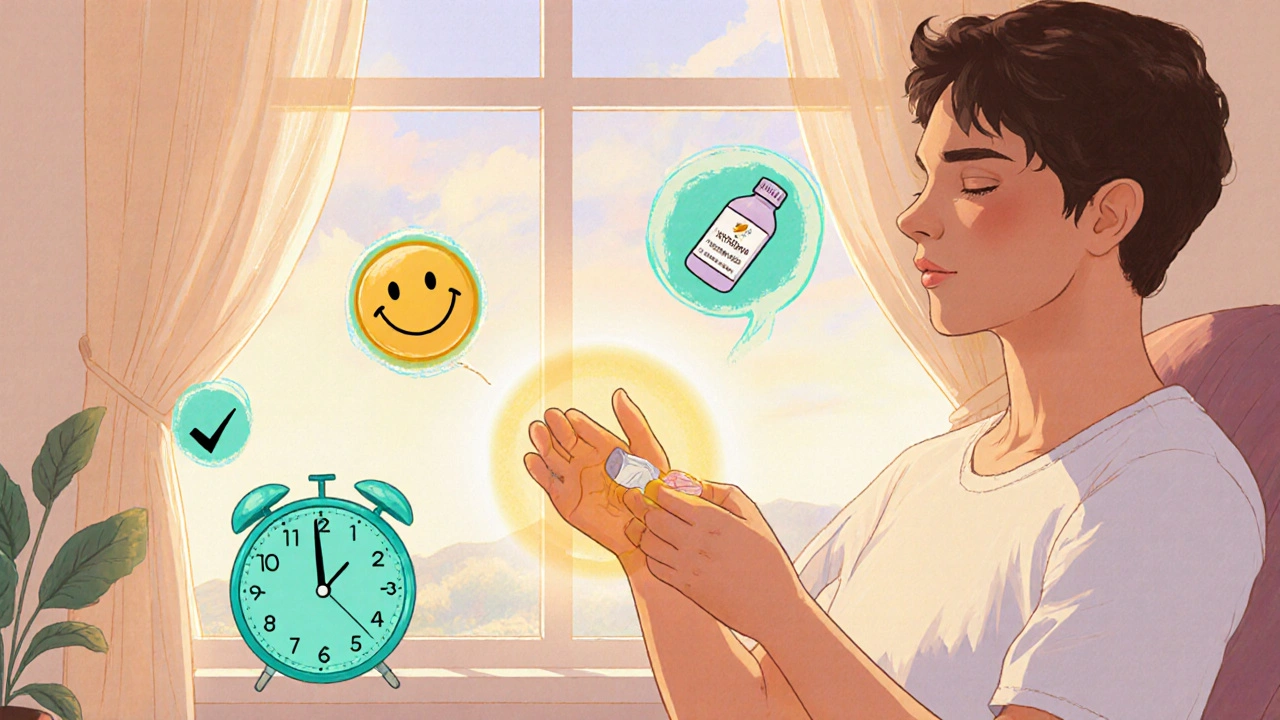
Tips for optimal use in clinical practice
- Check wound closure: Only apply once skin edges are approximated; open wounds may increase systemic uptake.
- Document dosage: Record the exact amount applied; over‑application is the most common cause of skin irritation.
- Combine wisely: If additional systemic analgesia is required, favour acetaminophen over another NSAID to avoid duplication.
- Educate patients: Explain the “burning” sensation is normal and short‑lived; advise them to report persistent redness.
- Monitor high‑risk groups: Elderly or renal‑impaired patients still need renal function checks, even with low systemic exposure.
Future directions - where the research is heading
Newer formulations are exploring a sustained‑release matrix that could keep therapeutic levels at the wound for up to 72 hours, potentially cutting the number of applications in half. Parallel studies are also looking at adding a low‑dose opioid‑like peptide to the gel to tackle breakthrough pain without systemic exposure.
Bottom line
If you need a fast‑acting, skin‑friendly option for post‑operative discomfort, the choline salicylate‑lignocaine combo offers both anti‑inflammatory and numbing benefits with a low systemic safety profile. Use it within the first two days after surgery, respect the dosing schedule, and keep an eye out for skin reactions. When applied correctly, it can shave off the need for extra oral analgesics and get patients back to feeling normal sooner.
Can I use choline salicylate lignocaine on open surgical wounds?
It’s safest on closed or partially closed wounds. Applying the gel to a fully open incision can increase systemic absorption and may delay healing. Clean, approximate the edges first, then apply a thin layer.
How often should I re‑apply the gel?
Every 4‑6 hours is typical. Do not exceed six applications in 24 hours unless a physician advises otherwise.
Is there any risk of allergic reaction?
Allergic reactions to lignocaine are rare but possible. Look for hives, swelling, or breathing difficulty. If any appear, stop the gel and seek medical help immediately.
Can I combine this gel with oral ibuprofen?
Yes, a low‑dose oral NSAID can be added for extra pain control, but avoid high‑dose ibuprofen to prevent duplicate salicylate exposure.
What should I do if the skin becomes red or itchy?
Mild redness is common and often resolves on its own. If itching intensifies or the area swells, discontinue use and apply a cool compress. Contact your surgeon if symptoms persist beyond 24 hours.