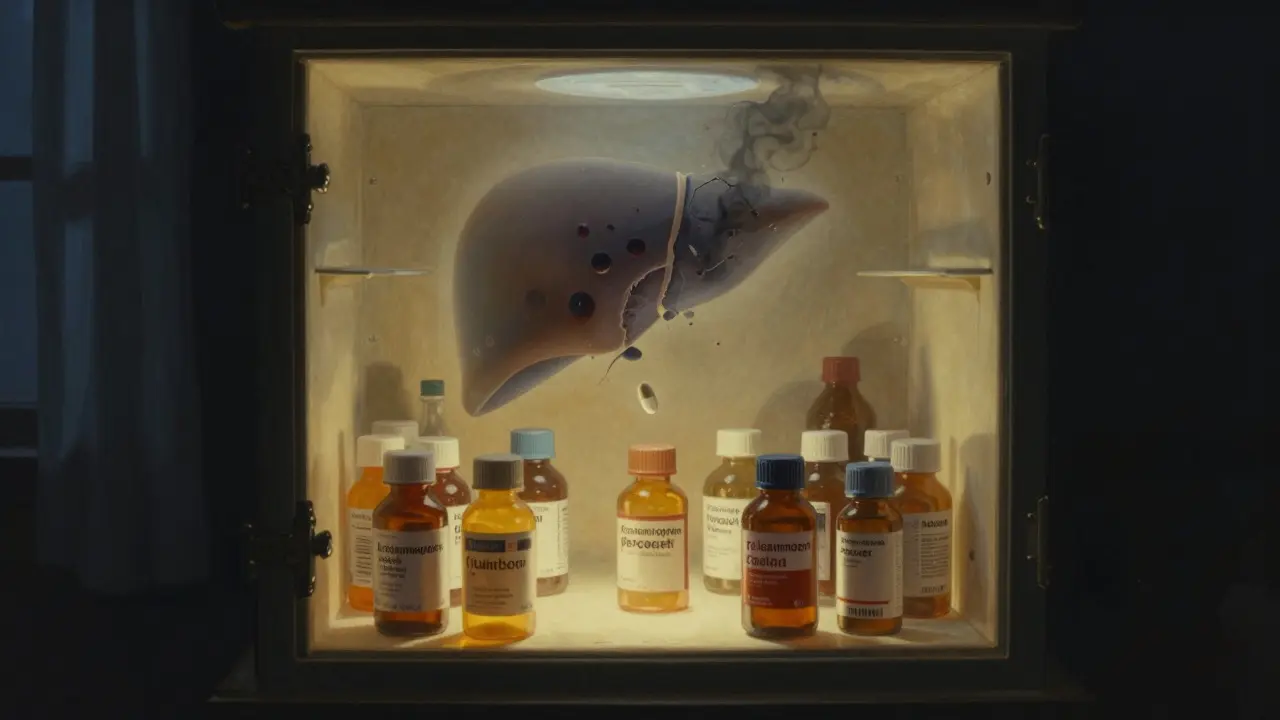
Acetaminophen is in almost every medicine cabinet - and it’s quietly dangerous
You take it for a headache. Your kid takes it for a fever. Your partner takes it for back pain. You grab a cold medicine that also has it. You think you’re being careful. But if you’re not watching the labels, you could be on track for a silent liver crisis - and you might not even feel sick until it’s too late.
Acetaminophen, also known as paracetamol or by the brand name Tylenol, is one of the most common pain relievers in the world. It’s in over 600 different medicines - from cold and flu blends to prescription opioids like Vicodin and Percocet. It’s safe when you use it right. But the line between safe and dangerous is thinner than most people realize. Take just a few extra pills over a day or two, and you could be staring at acute liver failure.
In the U.S. alone, acetaminophen causes more than 56,000 emergency room visits and 500 deaths every year. It’s the top reason for sudden liver failure in the country. And here’s the worst part: most of those cases aren’t from suicide attempts. They’re from people who didn’t know they were taking too much.
How acetaminophen damages your liver - and why you won’t feel it until it’s too late
Your liver breaks down acetaminophen into harmless parts. But when you take too much, the liver gets overwhelmed. It starts producing a toxic byproduct called NAPQI. Normally, your body neutralizes this with a molecule called glutathione. But when you overdose, glutathione runs out. NAPQI starts eating away at liver cells. And you won’t feel it - not right away.
The first 24 hours after an overdose? You might feel fine. Or maybe a little nauseous. A bit sweaty. You think, ‘It’s just a stomach bug.’ But inside your liver, cells are dying. By day two or three, you’ll start feeling real pain - sharp, deep, under your right ribs. Your skin turns yellow. You feel confused. Your blood won’t clot. That’s when you’re in the hospital, praying for a liver transplant.
There are four stages. Stage one: no symptoms. Stage two: your liver enzymes spike. Stage three: your organs start shutting down. Stage four: you either recover - or you don’t. And the window to save yourself? Just eight hours after taking too much.
What’s a safe dose? (Spoiler: it’s lower than you think)
The official maximum daily dose for adults is 4,000 milligrams. That’s eight 500mg tablets. Sounds like a lot, right? But here’s the catch: that’s the absolute ceiling. Most doctors now recommend staying under 3,000 mg per day - especially if you drink alcohol, have liver issues, or are older.
Here’s how easy it is to hit that limit without trying:
- Two extra-strength Tylenol (1,000 mg)
- Plus a cold medicine with 325 mg acetaminophen per tablet - you take two of those (650 mg)
- Plus a prescription painkiller like Percocet - each has 325 mg
- That’s already 2,000 mg in three hours.
By bedtime, you’re halfway to danger. And if you do it again the next day? You’re in overdose territory.
For kids, the rules are even stricter. Dose is based on weight: 10-15 mg per kilogram per dose. Never use adult pills for children. Never use kitchen spoons to measure liquid medicine. A tablespoon isn’t the same as a teaspoon - and 41% of pediatric overdoses happen because of this mistake.

The hidden danger: combination products
Acetaminophen doesn’t just hide in painkillers. It’s in nearly every multi-symptom cold and flu remedy. Look at the label. You’ll see ‘acetaminophen’ - tiny, in fine print. Or you’ll see ‘APAP’ - the chemical abbreviation. If you don’t know what that means, you’re not alone. Only 38% of people surveyed could identify it as the ingredient linked to liver damage.
People think: ‘I’m just taking this for my stuffy nose.’ But they’re not realizing they’re stacking doses. One study found that 25% of accidental overdoses happen because people take two or more acetaminophen-containing products at once.
And don’t forget prescription drugs. Vicodin, Norco, Percocet - they all contain acetaminophen. If you’re taking those for pain, you can’t also take Tylenol. Even if you’re not feeling well, even if you think ‘just one more’ won’t hurt. It will.
Alcohol makes it worse - even a little
If you drink alcohol regularly - even just one or two drinks a day - your liver is already under stress. It’s using up glutathione to break down the alcohol. Now add acetaminophen? You’re running out of protection faster. Studies show that people who drink regularly can develop liver damage from doses as low as 3,000 mg per day - well under the official limit.
Don’t think ‘I only have a glass of wine with dinner.’ That’s enough. If you’re taking acetaminophen, skip the alcohol. Full stop.
What to do if you think you’ve taken too much
If you realize you’ve taken more than you should - don’t wait. Don’t hope it’ll pass. Don’t Google symptoms. Call poison control immediately. In the U.S., it’s 1-800-222-1222. In Australia, call 13 11 26. In Canada, it’s 1-844-757-4777. These lines are staffed 24/7 by experts who know exactly what to do.
The antidote - N-acetylcysteine (NAC) - works best if given within eight hours. If you get it within that window, your chances of full recovery are over 90%. After 16 hours? That drops to 60%. And after 24? The risk of liver failure skyrockets.
One woman in Ohio took six extra-strength Tylenol for back pain. She felt fine for 12 hours. Then she vomited, turned yellow, and collapsed. Her liver enzymes were 12 times higher than normal. She got NAC 10 hours after taking the pills. She survived - but barely. She spent six weeks in the hospital. She’ll never take acetaminophen again.

How to prevent an overdose - simple, proven steps
Here’s what actually works:
- Always read the label. Look for ‘acetaminophen’ or ‘APAP’ on every medicine you take - even if it’s a new brand.
- Keep your daily total under 3,000 mg. Don’t max out at 4,000 unless your doctor says so.
- Never mix acetaminophen with alcohol. Not even one drink.
- Use the measuring tool that comes with liquid medicine. Never use a kitchen spoon.
- Ask your pharmacist. If you’re on multiple meds, ask: ‘Does any of this have acetaminophen?’
- Don’t take ‘extra strength’ unless you adjust your dose. One extra-strength tablet = two regular ones.
- Store medicines out of reach of kids. And never leave them on the nightstand where someone might grab them in the dark.
There’s no magic trick. Just awareness. Just discipline. Just treating acetaminophen like a powerful drug - because it is.
What’s changing? New warnings and better tools
The FDA is pushing for bigger, bolder ‘acetaminophen’ labels on all products. Some companies are already testing barcode-scanning apps that tell you your total daily dose as you scan each bottle. Poison control centers now use a standardized tool called the Rumack-Matthew nomogram to quickly assess overdose risk.
But the biggest change? Education. The American Liver Foundation found that 23% of adults didn’t know acetaminophen was the active ingredient in Tylenol. That’s not ignorance - it’s a system failure. Labels are too small. Abbreviations are too confusing. People aren’t warned clearly enough.
Until those labels change, you have to be your own watchdog.
Bottom line: acetaminophen is safe - if you respect it
It’s not the villain. It’s a lifesaver when used right. Millions of people take it every day without issue. But that doesn’t mean it’s harmless. It means you have to be smart.
If you’re taking more than one medicine, you’re playing Russian roulette with your liver. If you drink, you’re rolling the dice twice. If you don’t check labels, you’re blindfolded.
Don’t wait for symptoms. Don’t hope you’ll be fine. If you’re unsure, call poison control. If you’re taking acetaminophen, keep a written log of every dose. Write it down. It’s that simple.
Your liver doesn’t scream. It whispers. And if you ignore the whisper, it stops working.
Can I take acetaminophen if I have liver disease?
If you have liver disease - even mild fatty liver - you should only take acetaminophen under a doctor’s supervision. Most experts recommend limiting it to 2,000 mg per day or less. Some people with advanced disease need to avoid it entirely. Never assume it’s safe just because it’s over-the-counter.
Is Tylenol safer than ibuprofen?
It depends. Tylenol doesn’t irritate your stomach or raise blood pressure like ibuprofen can. That makes it better for people with ulcers, kidney issues, or heart conditions. But ibuprofen doesn’t cause liver failure. If you’re healthy and don’t drink, ibuprofen might be safer overall. If you have liver concerns, Tylenol is still preferred - but only if you stick to low doses.
What if I accidentally took too much but feel fine?
Feeling fine doesn’t mean you’re safe. Liver damage from acetaminophen often has no symptoms for 12 to 24 hours. If you took more than 7.5 grams in a day - or more than 150 mg per kg of body weight - call poison control immediately. Don’t wait. Don’t check symptoms online. Get help now.
Can children take adult Tylenol?
Never. Adult Tylenol tablets are 500 mg each. A child weighing 30 kg (about 66 lbs) should get no more than 450 mg per dose. Giving them an adult tablet could cause severe liver damage or death. Always use pediatric formulations and measure with the provided syringe or cup.
How long does acetaminophen stay in your system?
It takes about 2 to 4 hours for half of a dose to leave your body. Most of it is gone in 12 to 24 hours. But the damage it causes can take days to show up. That’s why waiting to act is so dangerous. The drug may be gone, but the toxic byproducts are still attacking your liver.
Is there a blood test to check for acetaminophen overdose?
Yes. Doctors can test your blood for acetaminophen levels, especially if you present within 24 hours of ingestion. They’ll use the Rumack-Matthew nomogram to plot your level against time and determine if you need NAC. Liver enzyme tests (AST, ALT) will also show damage - but those rise later, so they’re not the first line of detection.
Can I take acetaminophen while pregnant?
Yes - but only at the lowest effective dose for the shortest time. It’s considered the safest pain reliever during pregnancy, unlike NSAIDs like ibuprofen, which can affect fetal development. Still, don’t exceed 3,000 mg per day. Always check with your OB-GYN before taking any medication, even if it’s labeled ‘safe.’