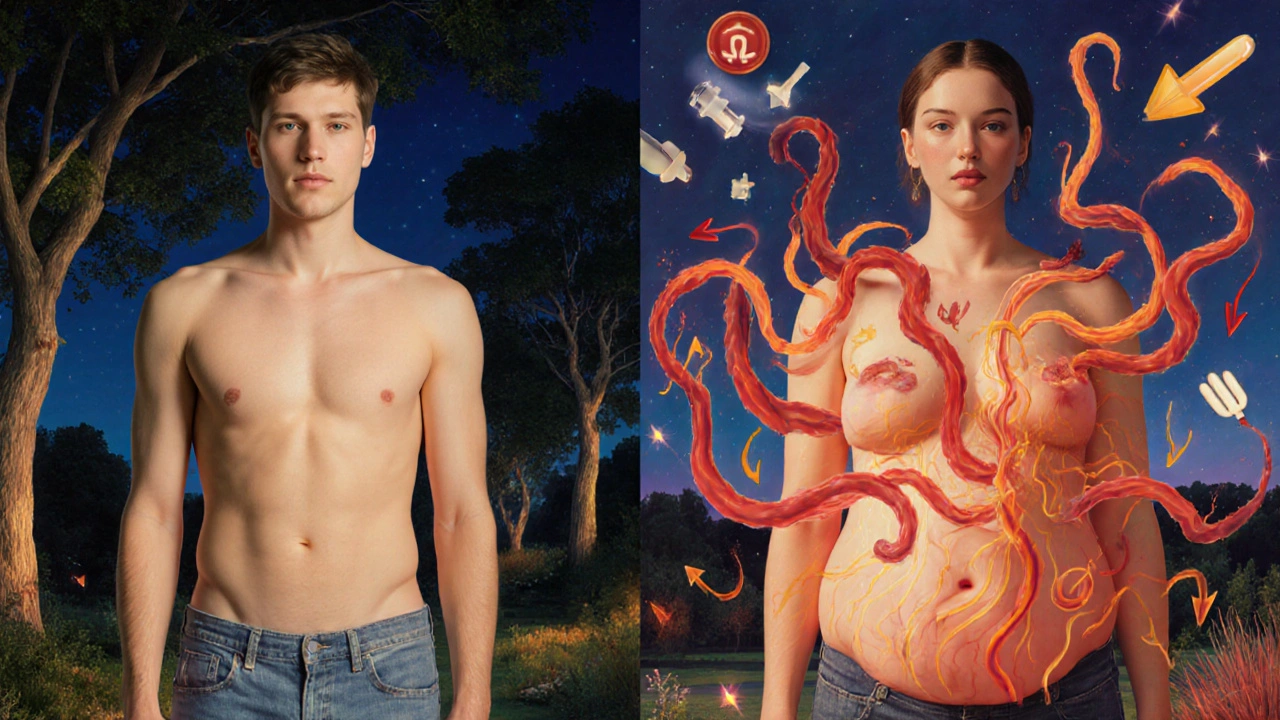
When your waistline keeps growing, your blood pressure creeps up, and your cholesterol numbers look like a warning sign - it’s not just bad luck. It could be metabolic syndrome. This isn’t one disease. It’s a cluster of five warning signs that work together to turn your body into a ticking time bomb for heart disease, stroke, and type 2 diabetes. And here’s the scary part: about one in three adults in the U.S. and Australia already have it - and most don’t even know.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t something you can see in a mirror or feel in your bones. There’s no pain, no fever, no cough. The only obvious clue? A big belly. But behind that visible sign are four hidden problems: high blood pressure, abnormal cholesterol levels, high blood sugar, and too much fat around your waist. You don’t need all five to be diagnosed. Just three out of these five are enough:
- Waist circumference over 102 cm (40 inches) for men, or 88 cm (35 inches) for women
- Triglycerides at 150 mg/dL or higher
- HDL cholesterol below 40 mg/dL for men, or 50 mg/dL for women
- Blood pressure at 130/85 mmHg or higher
- Fasting blood sugar of 100 mg/dL or above
These numbers come from guidelines set by the American Heart Association and the National Heart, Lung, and Blood Institute. Some organizations, like the International Diabetes Federation, put more weight on waist size - calling it the key trigger. Either way, the message is the same: if you’ve got three of these, your body is in metabolic chaos.
Why Abdominal Fat Is the Real Culprit
Not all fat is the same. Fat around your hips and thighs? That’s mostly storage. Fat around your belly - especially deep inside your abdomen, wrapped around your liver and organs? That’s active, dangerous tissue. These fat cells aren’t just sitting there. They’re pumping out chemicals that make your body resistant to insulin, raise inflammation, and mess with your blood vessels.
That’s why waist size matters more than total weight. Two people can weigh the same, but if one has a belly like a basketball and the other carries weight evenly, the one with the big waist is at far greater risk. Studies show that abdominal fat releases free fatty acids directly into the liver, which then spits out more triglycerides and makes HDL (the good cholesterol) drop. It’s a domino effect - and it starts right in your midsection.
How Blood Pressure and Lipids Connect
High blood pressure and bad cholesterol don’t just happen together by accident. They’re both symptoms of the same root problem: insulin resistance. When your muscles and liver stop responding to insulin, your body tries to compensate by making more of it. That extra insulin tells your kidneys to hold onto sodium, which raises your blood pressure. At the same time, it tells your liver to churn out more triglycerides and less HDL.
Think of it like a broken thermostat. Your body thinks it needs more energy, so it floods your bloodstream with sugar and fat. But your cells can’t use it properly. The result? Sugar piles up in your blood (leading to prediabetes), fat builds up in your arteries (raising heart disease risk), and your blood vessels get stiff and inflamed (spiking your pressure). It’s a self-reinforcing cycle - and it gets worse the longer it goes untreated.
Who’s at Risk - And Why It’s Getting Worse
Metabolic syndrome doesn’t pick favorites, but it does favor certain patterns. The risk jumps sharply after age 40. In Australia, more than 35% of adults have it. In the U.S., it’s about the same - and rising. Why? Three big reasons:
- Processed food: Sugary drinks, refined carbs, and trans fats overload your liver and trigger fat storage around your organs.
- Sitting too much: Even if you exercise, sitting 8+ hours a day slows down your metabolism and makes insulin less effective.
- Genetics and ethnicity: People of South Asian, Hispanic, African American, and Native American descent are more likely to develop metabolic syndrome at lower body weights.
Women with polycystic ovary syndrome (PCOS) are also at much higher risk - up to 70% of them show signs of metabolic syndrome. And it’s not just about weight. Even people who seem "skinny" can have hidden belly fat - a condition doctors call "TOFI" (thin outside, fat inside). That’s why waist measurement is more important than the scale.
There Are No Symptoms - Until It’s Too Late
This is why metabolic syndrome is so dangerous. It’s silent. You won’t feel it until your blood pressure spikes enough to cause a headache, or your blood sugar climbs high enough to make you thirsty and tired all the time. By then, damage may already be done.
Some people notice a dark, velvety patch on their neck or underarms - a sign called acanthosis nigricans. That’s often a red flag for insulin resistance. But most don’t see anything until they get a routine blood test or a doctor measures their waist and says, "This is too high." That’s when the real work begins.
How to Reverse It - No Pills Required
The good news? Metabolic syndrome is reversible - and you don’t need surgery or expensive drugs to fix it. The most effective treatment is simple, but not easy: lifestyle change.
Studies from Penn Medicine and the Cleveland Clinic show that losing just 5-10% of your body weight can cut your triglycerides by 20%, raise HDL by 10%, lower blood pressure by 5-10 points, and bring your blood sugar back into the normal range. That’s not magic. That’s biology.
Here’s what works:
- Move more: Aim for 150 minutes of brisk walking, cycling, or swimming each week. Even three 10-minute walks a day help. Strength training twice a week boosts muscle, which burns more sugar.
- Eat real food: Cut out sugary drinks, white bread, pastries, and fried snacks. Focus on vegetables, beans, whole grains, lean protein, nuts, and healthy fats like olive oil and avocado.
- Stop smoking: Smoking makes insulin resistance worse and damages your blood vessels on top of everything else.
- Sleep better: Poor sleep raises cortisol, which increases belly fat and blood sugar. Aim for 7-8 hours a night.
One 2023 study tracked 300 people with metabolic syndrome who followed a structured lifestyle program for 12 months. Two-thirds of them reversed their diagnosis. Not just improved - reversed. Their numbers went back to normal. No medication needed.

When Medication Becomes Necessary
Lifestyle is the foundation - but sometimes, you need extra help. If your blood pressure stays high after six months of change, your doctor might prescribe an ACE inhibitor or a calcium channel blocker. If your triglycerides are above 500 mg/dL or your HDL is dangerously low, statins or fibrates might be added. For blood sugar, metformin is often used to improve insulin sensitivity, even before full-blown diabetes develops.
But here’s the key: these drugs don’t cure metabolic syndrome. They manage the symptoms. Only lifestyle change fixes the root cause. Medication is a bridge - not a destination.
What Happens If You Ignore It?
Left unchecked, metabolic syndrome doesn’t just stay the same. It gets worse. Each component feeds the others:
- High blood sugar damages blood vessels → increases stroke risk
- Low HDL and high triglycerides cause plaque buildup → leads to heart attack
- Chronic inflammation from belly fat → triggers arthritis, fatty liver, even some cancers
Research published in Diabetes Care found that people with metabolic syndrome are twice as likely to have a heart attack or stroke compared to those without it. A 2022 meta-analysis of nearly 3 million people showed they’re five times more likely to develop type 2 diabetes. That’s not a small risk. That’s a life-altering one.
What to Do Next
If you’re over 40, carry extra weight around your middle, or have a family history of diabetes or heart disease - get checked. Ask your doctor for:
- A waist measurement
- A fasting blood test for glucose, triglycerides, and HDL
- A blood pressure reading
Don’t wait for symptoms. Don’t assume you’re fine because you’re not obese. Even if you’re "normal weight," a big waistline is a red flag.
Start small. Swap one sugary drink for water. Take a 15-minute walk after dinner. Park farther away. These tiny changes add up. And if you’ve already been diagnosed - don’t panic. You’re not doomed. You’re just at a turning point. The same habits that got you here are the ones that can save you.
Can you have metabolic syndrome and not be overweight?
Yes. Some people have what’s called "TOFI" - thin outside, fat inside. Their weight may be normal, but they carry dangerous fat deep in their abdomen. This is common in people with a family history of diabetes or those of South Asian descent. Waist measurement is the key indicator, not body weight.
Is metabolic syndrome the same as prediabetes?
No. Prediabetes means your blood sugar is higher than normal but not yet diabetic. Metabolic syndrome includes prediabetes as one of five possible components. You can have prediabetes without metabolic syndrome - and you can have metabolic syndrome without prediabetes if you have three other risk factors.
Does everyone with a big belly have metabolic syndrome?
No. A large waist is a major red flag, but you need at least two other factors - like high triglycerides, low HDL, high blood pressure, or high blood sugar - to be diagnosed. Still, if your waist is over the limit, you’re at high risk. Get tested.
Can children get metabolic syndrome?
Yes. With rising childhood obesity, metabolic syndrome is now seen in teens and even younger kids. The same criteria apply, adjusted for age and sex. Early signs include dark skin patches, high blood pressure, and abnormal blood fats. Prevention through healthy eating and activity is critical.
Will losing weight fix everything?
Losing 5-10% of your body weight typically improves all five markers of metabolic syndrome. But it’s not just about the number on the scale. Where you lose fat matters most. Belly fat shrinks first with diet and exercise, and that’s what lowers your risk fastest. Even small losses make a big difference.
If you’re reading this and thinking, "That’s me," you’re not alone. And you’re not too late. Metabolic syndrome is a wake-up call - not a death sentence. The tools to fix it are simple, proven, and within reach. Start today. Your heart, liver, and future self will thank you.

