When you leave the hospital, your medication plan often changes. Maybe you stopped taking a blood thinner while inpatient. Maybe you were started on a new antibiotic. Or perhaps your dose for high blood pressure was adjusted. But here’s the problem: medication reconciliation-the process of making sure your home meds match what was prescribed at discharge-isn’t automatic. And if it doesn’t happen, you’re at serious risk.
Studies show that 30% to 70% of patients leave the hospital with a medication list that doesn’t match what they were actually taking before admission. That mismatch causes up to half of all medication errors in the first 30 days after discharge. Some of these errors lead to emergency room visits. Others lead to hospital readmissions. And readmissions cost the U.S. healthcare system over $21 billion a year.
So how do you make sure your meds are right after you go home? It’s not just about getting a new list. It’s about coordination-between hospital staff, your primary care doctor, your pharmacist, and you.
What Medication Reconciliation Actually Means
Medication reconciliation isn’t a one-time form you sign. It’s a process. The National Quality Forum calls it NQF 0097, and the Centers for Medicare & Medicaid Services (CMS) requires it. The goal is simple: compare your current medications with your discharge medications to find any mismatches.
That means checking:
- What you were taking before you went to the hospital
- What you were given while you were there
- What you’re supposed to take when you go home
It’s not just pills. It includes patches, eye drops, creams, vitamins, supplements, and even herbal teas. If you were taking ashwagandha for sleep and the hospital didn’t note it, that could interact with your new blood pressure med. If you stopped your warfarin for surgery and no one told your doctor to restart it, you could develop a clot.
According to the American Society of Health-System Pharmacists (ASHP), this process must be documented clearly in your outpatient chart. The documentation has to show one of seven things: that the provider reviewed both lists, that they reconciled them, that they noted no changes, or that follow-up occurred within 30 days. If it’s not documented, it didn’t happen.
The Two Main Ways It’s Done (And Why One Works Better)
There are two common ways hospitals and clinics handle this after discharge.
The first is the CPT II code 1111F. This lets your doctor or nurse document reconciliation without you even coming in. They can call you, video chat, or review your EHR records. No office visit needed. But here’s the catch: insurance doesn’t pay for this. So many providers skip it because it takes time and brings no money.
The second is the Transitions of Care (TRC) visit, billed under CPT 99495 or 99496. This requires an in-person appointment within 30 days of discharge. You see your doctor, they review your meds, and they get paid for it. Sounds good, right?
But there’s a major flaw: only one TRC visit can be billed per discharge. That means if you’re seeing a cardiologist, a neurologist, and your primary care doctor, only one of them can get paid. The others have no financial incentive to do the work. So who ends up doing it? Often, no one. Or worse-the wrong person.
Research from the Journal of the American College of Clinical Pharmacy in 2023 found that when pharmacists lead the reconciliation, medication errors drop by 32.7%. Readmissions drop by 28.3%. Why? Because pharmacists specialize in drugs. They know interactions. They know how to ask the right questions. They’re trained to dig into your actual use-not just what’s written on paper.
One study showed that when pharmacists were embedded in hospital discharge teams, medication discrepancies fell by 37%. They don’t just check lists-they call you. They ask: “Did you fill that new prescription?” “Are you taking your insulin like you were told?” “Did your wife stop your old blood pressure pill because she thought it was making you dizzy?”
Why Your Doctor Might Not Catch the Mistake
It’s not that your doctor doesn’t care. It’s that they’re overwhelmed.
Specialists focus on one thing. A cardiologist is worried about your stent. A rheumatologist is focused on your arthritis flare. They don’t always look at your full list. If you were on a blood thinner before admission and it was stopped for surgery, they might not realize it was never restarted. And if your primary care doctor didn’t get a clear handoff, they won’t know either.
The NIH gives a real example: a patient had warfarin stopped during a hospital stay for bleeding. When discharged, no one restarted it. Three weeks later, they had a stroke. Why? Because no one checked the full history.
And here’s another hidden issue: electronic health records (EHRs) don’t talk to each other. A hospital system might use Epic. Your primary care clinic uses Cerner. Your pharmacy uses a different system. Information gets lost in translation. A 2022 AHRQ survey found that 68% of hospitals reported fragmented EHRs as a major barrier to accurate reconciliation.
What You Can Do (Before and After Discharge)
You’re not powerless. You can take control.
Before you leave the hospital:
- Ask for a printed list of all your discharge medications. Don’t rely on memory.
- Ask: “What changed from what I was taking before I came in?” Write it down.
- Ask: “Is this list shared with my primary care doctor?” If not, ask them to send it.
- Bring a list of everything you were taking at home-including vitamins, supplements, and over-the-counter drugs.
Right after discharge:
- Call your pharmacy and ask them to review your new prescriptions. Pharmacists are trained to catch interactions.
- Set a calendar reminder: “Call my doctor in 5 days” to confirm you got the right meds.
- If you’re supposed to start a new pill but can’t find it at the pharmacy, don’t assume it’s a mistake. Call your doctor’s office. Many prescriptions get delayed because the insurance didn’t approve it.
Within 30 days:
- Make sure you have a follow-up visit. If you’re not scheduled, call your PCP and ask for one.
- Bring your full medication list-not just the discharge sheet. Include pill bottles.
- Ask: “Did you get my discharge summary? Did you compare my old meds with my new ones?”
If your doctor says they didn’t receive it, ask them to request it from the hospital. Most hospitals are required to send discharge summaries within 24-48 hours. If they didn’t, it’s a system failure-and you’re the one paying for it.
How Technology Is Helping (And Where It Still Falls Short)
Some hospitals are using AI tools to flag discrepancies. A 2022 JAMIA study found AI could predict potential errors with 87% accuracy by scanning EHRs for patterns: a patient on statins suddenly stopped, new anticoagulant added, no documentation of review.
Mobile apps are also helping. Patients in top-performing hospitals use apps to take photos of their pill bottles and upload them. The system matches them with the discharge list. If there’s a mismatch, a pharmacist gets notified.
But tech alone doesn’t fix the problem. You still need a person to verify. A 2023 study showed that even with AI, 41% of discrepancies were only caught when pharmacists directly called the patient and asked: “Are you actually taking this?”
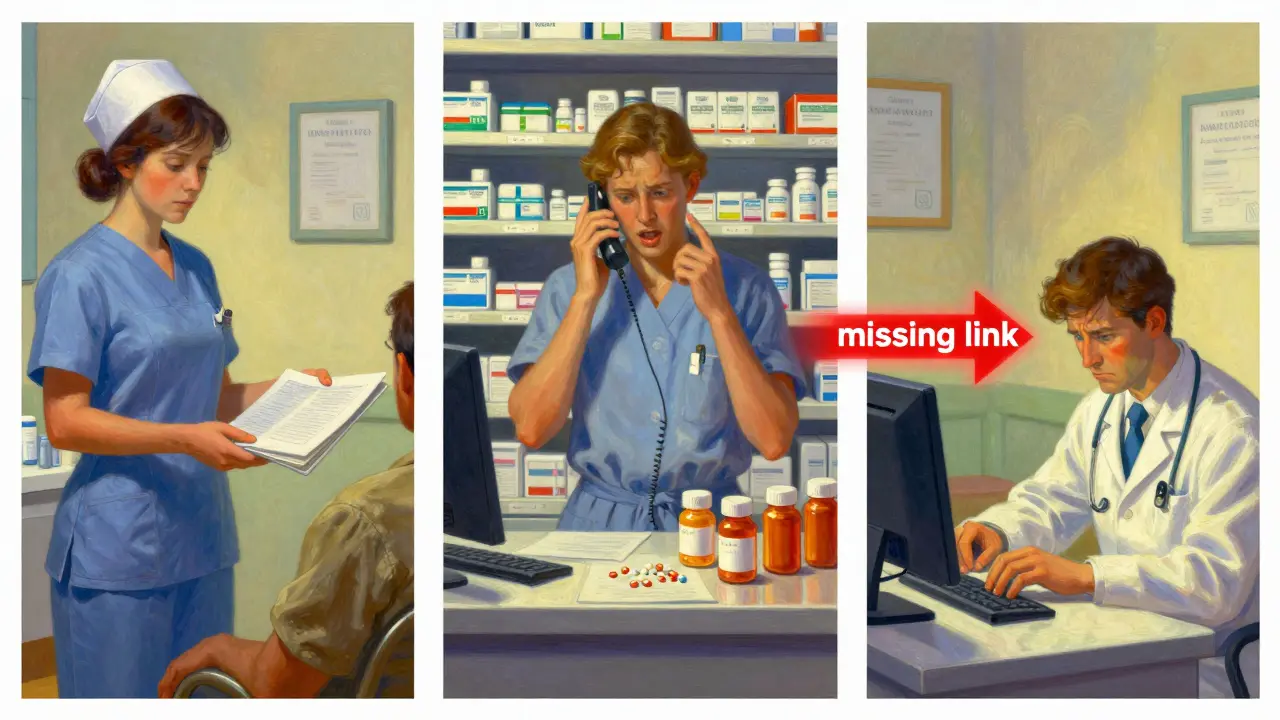
That’s the missing piece: confirmation of adherence. Just because a drug is prescribed doesn’t mean it’s taken. Up to 50% of patients don’t fill their discharge prescriptions. Some can’t afford them. Others are confused. Some are scared of side effects. A pharmacist calling to ask “How’s the new pill working?” can uncover issues no algorithm can.

Who Should Be in Charge?
Who’s responsible for reconciliation? Legally, it’s the provider who sends the discharge summary. But practically? It should be the person with the most expertise in medications.
That’s the pharmacist.
Yet most hospitals still rely on nurses or doctors to do it. Why? Because billing rules make it hard to pay pharmacists for this work. But that’s changing. Medicare Advantage plans now cover post-discharge medication therapy management. And by 2026, 75% of hospitals are expected to have pharmacist-led programs-up from just 48% in 2023.
Don’t wait for the system to fix itself. If your hospital doesn’t have a pharmacist on the discharge team, ask why. If your primary care doctor doesn’t mention reconciliation at your first follow-up, ask: “Did you get my discharge meds list? Did you compare it?”
The Bottom Line
Medication reconciliation isn’t paperwork. It’s a safety net. And right now, that net has holes.
The data is clear: pharmacist-led reconciliation cuts errors and readmissions. Documentation matters. Communication matters. And you matter.
Don’t assume your meds are right after discharge. Double-check. Ask questions. Bring your pill bottles. Call your pharmacist. Push for a follow-up. If no one else is doing it, you have to be the one.
Because in the first 30 days after the hospital, your life could depend on it.
What happens if my discharge meds don’t match what I was taking before the hospital?
If your discharge meds don’t match your pre-hospital list, you’re at risk for serious harm. You might take a drug you’re allergic to, miss a critical medication like an anticoagulant, or double-dose on something you were already taking. This mismatch causes up to 50% of medication errors after discharge. Always ask for a side-by-side comparison and keep a written list.
Can my specialist and my primary care doctor both bill for medication reconciliation after my hospital stay?
No. Medicare and most insurers only allow one Transitions of Care (TRC) visit to be billed per discharge. This creates a conflict: both providers may need to do the work, but only one gets paid. As a result, many patients get passed between doctors without clear accountability. That’s why pharmacist-led reconciliation-done outside billing constraints-is often more effective.
Is medication reconciliation required by law?
Yes. The Centers for Medicare & Medicaid Services (CMS) requires it as part of the National Quality Forum measure NQF 0097. Hospitals must document reconciliation for patients discharged to outpatient care. Failure to report can reduce physician reimbursement by up to 9% under CMS’s Merit-based Incentive Payment System (MIPS). But documentation doesn’t always mean action-so you still need to verify it happened.
Why do I need to see my doctor within 30 days after discharge?
The 30-day window is the standard timeframe for medication reconciliation to be considered complete. This is when most errors occur-patients forget to fill prescriptions, side effects appear, or insurance denies coverage. A follow-up visit gives your provider a chance to catch problems before they lead to an ER visit or readmission. Even if you feel fine, don’t skip it.
Can my pharmacist help even if I didn’t get a follow-up appointment?
Yes. Pharmacists are trained to review medication histories and catch discrepancies. Bring your pill bottles to the pharmacy and ask them to compare your discharge list with what you’re actually taking. Many pharmacies now offer free post-discharge medication reviews. This is especially important if you’re on five or more medications, have kidney or liver disease, or are over 65.

